Abstract
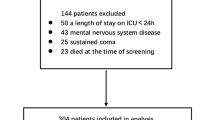
Delirium is a common postoperative complication in children with congenital heart disease, which affects their postoperative recovery. The purpose of this study is to explore the risk factors of delirium and construct a nomogram model to provide novel references for the prevention and management of postoperative delirium in children with congenital heart disease. 470 children after congenital heart surgery treated in the cardiac intensive care unit (CICU) of Shanghai Children’s Medical Center were divided into a model and a validation cohort according to the principle of 7:3 distribution temporally. Then, the delirium-related influencing factors of 330 children in the training cohort were analyzed, and the nomogram model was established by a combination of Lasso regression and logistic regression. The data of 140 children in the validation cohort were used to verify the effectiveness of the model. Multivariable logistic regression analysis showed that age, disease severity, non-invasive ventilation after extubation, delayed chest closure, phenobarbital dosage, promethazine dosage, mannitol usage, and elevated temperature were independent risk factors for postoperative delirium. The area under the receiver operating characteristic curve (AUC) of the nomogram model was 0.864 and the Brier value was 0.121. Regarding the validation of the model’s effect, our results showed that 51 cases were predicted by the model and 34 cases actually occurred, including 4 cases of false negative and 21 cases of false positive. The positive predictive value of the model was 58.8%, and its negative predictive value was 95.5%. The nomogram model established in this study showed acceptable performance in predicting postoperative delirium in children with congenital heart disease.







Similar content being viewed by others
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- CICU:
-
Cardiac intensive care unit
- AUC:
-
Area under the receiver operating characteristic curve
- RASS:
-
Richmond agitation-sedation scale
- CAPD:
-
Cornell assessment of pediatric delirium
- EMR:
-
Electronic medical records
- ROC:
-
Receiver operating characteristic
- PICU:
-
Pediatric intensive care unit
- ICU:
-
Intensive care unit
- CI:
-
Confidence interval
- RACHS-1:
-
Risk heart adjustment for congenital surgery-1
- STS-EACTS:
-
The Society of Thoracic Surgeons and the European Association for Cardiothoracic Surgery Congenital Heart Surgery Mortality Score
- PRISM III:
-
Pediatric risk of mortality III
References
Hoffman J (2013) The global burden of congenital heart disease. Cardiovasc J Afr 24:141–145
Alvarez RV, Palmer C, Czaja AS, Peyton C, Silver G, Traube C, Mourani PM, Kaufman J (2018) Delirium is a common and early finding in patients in the pediatric cardiac intensive care unit. J Pediatr 195:206–212
Patel AK, Biagas KV, Clarke EC, Gerber LM, Mauer E, Silver G, Chai P, Corda R, Traube C (2017) Delirium in children after cardiac bypass surgery. Pediatr Crit Care Med 18:165–171
Staveski SL, Pickler RH, Khoury PR, Ollberding NJ, Donnellan AL, Mauney JA, Lincoln PA, Baird JD, Gilliland FL, Merritt AD, Presnell LB, Lanese AR, Lisanti AJ, Large BJ, Fineman LD, Gibson KH, Mohler LA, Callow L, Barnes SS, Whalen RL, Grant MJC, Sheppard C, Kline-Tilford AM, Steadman PW, Shafland HC, Corlett KM, Kelly SP, Ortman LA, Peyton CE, Hagstrom SK, Shields AM, Nye T, Alvarez TCE, Justice LB, Kidwell ST, Redington AN, Curley MAQ (2020) Prevalence of ICU delirium in postoperative pediatric cardiac surgery patients. Pediatr Crit Care Med 22:68
Dervan LA, Di Gennaro JL, Farris RWD, Watson RS (2020) Delirium in a tertiary PICU: risk factors and outcomes. Pediatr Crit Care Med 21:21–32
Traube C, Mauer EA, Gerber LM, Kaur S, Joyce C, Kerson A, Carlo C, Notterman D, Worgall S, Silver G, Greenwald BM (2016) Cost associated with pediatric delirium in the ICU. Crit Care Med 44:e1175–e1179
Silver G, Doyle H, Hegel E, Kaur S, Mauer EA, Gerber LM, Traube C (2020) Association between pediatric delirium and quality of life after discharge. Crit Care Med. 48:1829
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 350:g7594
Cano Londoño EM, Mejía Gil IC, Uribe Hernández K, Alexandra Ricardo Ramírez C, Álvarez Gómez ML, Consuegra Peña RA, Agudelo Vélez CA, Zuluaga Penagos S, Elorza Parra M, Franco Vásquez JG (2018) Delirium during the first evaluation of children aged five to 14 years admitted to a paediatric critical care unit. Intensive Crit Care Nurs 45:37–43
Trogrlić Z, van der Jagt M, Lingsma H, Gommers D, Ponssen HH, Schoonderbeek JFJ, Schreiner F, Verbrugge SJ, Duran S, Bakker J, Ista E (2019) Improved guideline adherence and reduced brain dysfunction after a multicenter multifaceted implementation of ICU delirium guidelines in 3930 patients. Crit Care Med 47:419–427
Trogrlić Z, van der Jagt M, Bakker J, Balas MC, Ely EW, van der Voort PH, Ista E (2015) A systematic review of implementation strategies for assessment, prevention, and management of ICU delirium and their effect on clinical outcomes. Crit Care 19:157
Paterson RS, Kenardy JA, De Young AC, Dow BL, Long DA (2017) Delirium in the critically Ill child: assessment and sequelae. Dev Neuropsychol 42:387–403
Malas N, Brahmbhatt K, McDermott C, Smith A, Ortiz-Aguayo R, Turkel S (2017) Pediatric delirium: evaluation, management, and special considerations. Curr Psychiatry Rep 19:65
Ista E, van Beusekom B, van Rosmalen J, Kneyber MCJ, Lemson J, Brouwers A, Dieleman GC, Dierckx B, de Hoog M, Tibboel D, van Dijk M (2018) Validation of the SOS-PD scale for assessment of pediatric delirium: a multicenter study. Crit Care 22:309
Meyburg J, Dill ML, Traube C, Silver G, von Haken R (2017) Patterns of postoperative delirium in children. Pediatr Crit Care Med 18:128–133
Zuppa AF, Curley MAQ (2017) Sedation analgesia and neuromuscular blockade in pediatric critical care: overview and current landscape. Pediatr Clin N Am 64:1103–1116
Kalvas LB, Harrison TM (2020) State of the science in pediatric ICU delirium: an integrative review. Res Nurs Health 43:341–355
Elassal AA, Eldib OS, Dohain AM, Abdelmohsen GA, Abdalla AH, Al-Radi OO (2019) Delayed sternal closure in congenital heart surgery: a risk-benefit analysis. Heart Surg Forum 22:E325-e330
Özker E, Saritaş B, Vuran C, Yörüker U, Ulugöl H, Türköz R (2012) Delayed sternal closure after pediatric cardiac operations; single center experience: a retrospective study. J Cardiothorac Surg 7:102
Smith HAB, Gangopadhyay M, Goben CM, Jacobowski NL, Chestnut MH, Thompson JL, Chandrasekhar R, Williams SR, Griffith K, Ely EW, Fuchs DC, Pandharipande PP (2017) Delirium and benzodiazepines associated with prolonged ICU stay in critically Ill infants and young children. Crit Care Med 45:1427–1435
Holly C, Porter S, Echevarria M, Dreker M, Ruzehaji S (2018) CE: original research: recognizing delirium in hospitalized children: a systematic review of the evidence on risk factors and characteristics. Am J Nurs 118:24–36
Mody K, Kaur S, Mauer EA, Gerber LM, Greenwald BM, Silver G, Traube C (2018) Benzodiazepines and development of delirium in critically Ill children: estimating the causal effect. Crit Care Med 46:1486–1491
Jiang L, Ding S, Yan H, Li Y, Zhang L, Chen X, Yin X, Liu S, Tang X, Zhang J (2015) A retrospective comparison of dexmedetomidine versus midazolam for pediatric patients with congenital heart disease requiring postoperative sedation. Pediatr Cardiol 36:993–999
Pan W, Wang Y, Lin L, Zhou G, Hua X, Mo L (2016) Outcomes of dexmedetomidine treatment in pediatric patients undergoing congenital heart disease surgery: a meta-analysis. Paediatr Anaesth 26:239–248
Riker RR, Shehabi Y, Bokesch PM, Ceraso D, Wisemandle W, Koura F, Whitten P, Margolis BD, Byrne DW, Ely EW, Rocha MG (2009) Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA 301:489–499
Kang X, Tang X, Yu Y, Bao F, Gan S, Zheng W, Zhang J, Zhu S (2019) Intraoperative dexmedetomidine infusion is associated with reduced emergence agitation and improved recovery profiles after lung surgery: a retrospective cohort study. Drug Des Devel Ther 13:871–879
Simonini A, Brogi E, Conti G, Vittori A, Cascella M, Calevo MG (2021) Dexmedetomidine reduced the severity of emergence delirium and respiratory complications, but increased intraoperative hypotension in children underwent tonsillectomy. A retrospective analysis. Minerva Pediatr (Torino). https://doi.org/10.23736/s2724-5276.21.06330-8
Motta E, Luglio M, Delgado AF (1992) Carvalho WB (2016) Importance of the use of protocols for the management of analgesia and sedation in pediatric intensive care unit. Rev Assoc Med Bras 62:602–609
Ming-lei WHL (2011) Diagnosis and emergency treatment of intracranial hypotension syndrome in children. Chin Pediatr Emerg Med 18:400–402
Zl F (2012) Clinical analysis of 15 children with intracranial hypotension syndrome. Matern Child Health Care China 27:634–635
Yu XQ (2010) Clinical analysis of intracranial hypotension syndrome in 35 infants. Clin Misdiagn Misther 23:441–443
Mu DL, Wang DX, Li LH, Shan GJ, Li J, Yu QJ, Shi CX (2010) High serum cortisol level is associated with increased risk of delirium after coronary artery bypass graft surgery: a prospective cohort study. Crit Care 14:R238
Patel AK, Biagas KV, Clark EC, Traube C (2017) Delirium in the pediatric cardiac extracorporeal membrane oxygenation patient population: a case series. Pediatr Crit Care Med 18:e621–e624
Acknowledgements
Our team would like to thank the staff and all the nurses who assisted in the investigation. We also would like to show our appreciation to the CICU team for supporting our research team. This research was funded by the Research Project on Science and Technology Innovation Think Tank of Fujian Science and Technology Association (FJKX-A2131) and Nursing discipline construction project of Shanghai Jiao Tong University School of Medicine (SJTUHLXK2021).
Funding
Research Project on Science and Technology Innovation Think Tank of Fujian Science and Technology Association, FJKX-A2131, FJKX-A2131, Nursing discipline construction project of Shanghai Jiao Tong University School of Medicine, SJTUHLXK2021.
Author information
Authors and Affiliations
Contributions
(I) Conception and design: DM, LF; (II) Administrative support: LF; (III) Provision of study materials or patients: LF; (IV) Collection and assembly of data: DM and WZ; (V) Data analysis and interpretation: DM and WZ; (VI) Manuscript writing: all authors; (VII) Final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mao, D., Fu, L. & Zhang, W. Risk Factors and Nomogram Model of Postoperative Delirium in Children with Congenital Heart Disease: A Single-Center Prospective Study. Pediatr Cardiol 45, 68–80 (2024). https://doi.org/10.1007/s00246-023-03297-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-023-03297-5