Abstract
A fetal cardiology consultation involves using two-dimensional drawings to explain the cardiac anatomy which can result in inherent variation in how the congenital heart disease (CHD) is conveyed. In this pilot study, we incorporated three-dimensional printed (3DP) models into fetal counseling to demonstrate feasibility and evaluate the impact on parental knowledge, understanding, and anxiety. Parents with a prenatal diagnosis of a muscular ventricular septal defect (VSD) and/or coarctation of aorta were enrolled. Providers were randomized into a Model or Drawing Group and crossed after six months. Parents completed a survey after the consultation which evaluated knowledge of the CHD lesion, expectant surgical management, self-rated understanding, attitude towards the visualization tool, and anxiety. Twenty-nine patients enrolled over a 12 month period. Twelve consultations were done for coarctation of aorta, 13 for VSD, and four for coarctation with a VSD. Both Model and Drawing groups scored similarly in self-reported understanding and confidence, helpfulness of and improvement in communication with the visualization tool. The Model group had higher scores on questions related to the CHD anatomy and surgical intervention [5 [4–5] versus 4 [3.5–5]], p = 0.23 although this didn’t reach statistical significance. For the majority (83%) of consultations, the cardiologist agreed that the 3D model improved communication. In this pilot study, we demonstrate the use of 3DP cardiac models during prenatal CHD counseling is feasible and produces results related to parental understanding and knowledge that are equal to and possibly better than the current standard of care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital heart disease (CHD) affects approximately 1 in every 100 live births in the US [1]. Up to 75% of complex lesions are diagnosed prenatally [2]. A prenatal diagnosis of CHD typically involves multiple visits with the family prior to their child’s birth. Each prenatal visit offers the opportunity for additional parental counseling and family education.
Routine prenatal counseling involves the fetal cardiologist explaining the CHD lesion using two-dimensional (2D) drawings. These diagrams are typically hand drawn and inevitably vary in style and quality from provider to provider. They are limited in representation of true spatial anatomy of the heart and have inherent variation due to different levels of skill in recreating three-dimensional cardiac anatomy in a 2D drawing. Three-dimensional printing (3DP) technology allows creation of 3DP models of specific CHD pathologies [3]. Such models provide a more concrete way to demonstrate spatial relationships between cardiac structures and serve as visualization tools which are standardized between providers. The utility of 3DP cardiac models in pediatric cardiology has been demonstrated in preprocedural planning and in medical education [4,5,6,7,8,9,10,11,12]. Although there is some literature on the utility of 3DP cardiac models as an aid in physician–patient communication, no studies have specifically focused on fetal counseling [13,14,15,16].
Literature demonstrates that a prenatal diagnosis of CHD is associated with parental stress, depression, and anxiety [17,18,19,20,21,22]. In this study, we aimed to investigate the feasibility and effectiveness of incorporating 3DP cardiac models of CHD lesions into fetal counseling. We also evaluated the impact of 3DP cardiac models on parental knowledge, understanding, and anxiety.
Materials and Methods
Model Creation
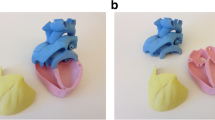
This study was approved by the Columbia University Irving Medical Center Institutional Review Board. We selected coarctation of the aorta and muscular ventricular septal defect (VSD) as the two congenital lesions to be included in our study, given that these are two of the most common lesions for which we provide fetal CHD counseling. Representative cardiac computed tomography (CT) scans done in older children were chosen to create the generic 3D models of these two lesions. Cardiac CT images for both lesions were loaded into Mimics software (Materialise, Belgium) and post processed to isolate the area of interest by segmentation using a previously established technique [23]. After segmentation, a preliminary 3D virtual model was created, which was edited to exclude extra-cardiac structures. A 1 mm-thick layer was created onto the 3D object which represented the blood pool. The 3D object was then “hollowed” internally, excluding the 1 mm layer, allowing for the intra-cardiac anatomy to be represented [24]. The myocardium was also segmented for the VSD model. This object was cropped to best demonstrate the relevant anatomic relationships and subsequently stored as a stereolithography file (STL). The STL files were processed on a Uprint SE printer (Stratasys, Eden Prairie, MN) to create a 3D physical model. The approximate cost of the cardiac model creation and printing was $55. The models used are shown in Fig. 1.
Three dimensional printed models used in the study. A Representative two dimensional (left) and color Doppler image (center) of a ventricular septal defect (red circle) from a fetal echocardiogram. The cropped 3D printed printed model is on the right, with the site of a midmuscular defect indicated by the red arrow. B Representative two dimensional (left) and color Doppler image (center) of coarctation of the aorta (red circle) from a fetal echocardiogram. The 3D printed model is on the right, with the site of the coarctation indicated by the red circle. Ao Aorta, PA pulmonary artery, LV left ventricle, RV right ventricle
Study Cohort and Design
Parents with a child with the prenatal diagnosis of suspected coarctation of the aorta and/or muscular VSD who underwent an initial fetal echocardiogram at NewYork-Presbyterian Morgan Stanley Children’s Hospital were approached to enroll over a 12 month period. Parents who were able to understand surveys in English or Spanish were included. Counseling sessions for Spanish speaking patients were completed using an in-person interpreter. There are eight fetal cardiologists who participated. To account for differences in provider practice and counseling style, we randomized half of the providers to a ‘Model group’ while the other half were assigned to a ‘Drawing group’. The providers crossed over to the other group halfway through study enrollment. This prospective cross-over model study design is represented in Fig. 2. The patient assignments to the ‘Model group’ and ‘Drawing group’ were made when a fetus with the inclusion diagnoses was seen. The group assignments were subject to the nature of random scheduling and to the provider that was engaging in fetal counselling that day.
Parents in the ‘Drawing group’ were counseled with only a standardized 2D drawing while the ‘Model group’ was counseled using a standardized 2D drawing and a 3DP model. When patients were enrolled in the study, the providers engaging in counseling used the same standardized 2D drawings in their sessions, which were printed ahead of time and provided by the study team. In cases where the cardiac anatomy differed minimally from the 2D drawing or 3DP model such as overall size of the ventricular septal defect, this was verbally explained to the parents by the provider.
Survey
After the fetal echocardiogram and parental counseling were complete, the parent was asked to complete the survey. The parental response was completed by one parent, either mother or partner. In our cohort, the parental response ended up being only from mothers due to majority of patient enrollment taking place during the COVID-19 pandemic. The survey contained three sections. The first section focused on parental knowledge and included five questions regarding the CHD lesion and potential surgical interventions needed postnatally. The questions related to understanding on our survey tool were modified from a validated survey tool previously utilized in a study assessing medical student understanding after exposure to 3D-printed models [10]. This section was given a total score that ranged from 0 to 5 based on the number of questions answered correctly. The second section was comprised of questions whereby parents self-rated their own level of understanding of the CHD, confidence in ability to explain the CHD, helpfulness of the 2D diagram and 3DP model, and improvement in communication using these visualization tools on a Likert scale (1–10) from least to most agreement. The third section included a standardized anxiety screening tool comprised of the 7-item Generalized Anxiety Disorder module (GAD-7) to assess parental anxiety [25]. GAD-7 total score ranges from 0 to 21. A score < 5 indicates minimal anxiety, 5–10 mild anxiety, 10–15 moderate anxiety, and > 15 severe anxiety. Parental demographics including age, gender, race, education level, marital status, household income, living environment, history of prior pregnancies/children, prior experience with CHD, and prior work in the medical field were also collected. A short six question survey was also administrated to the cardiologist after consultations done with the Model to gauge perceptions of counselling with addition of a 3D model. All surveys were either administered in person on paper or electronically using Qualtrics, an electronic survey program, which allows each survey to be securely distributed by QR code or by email.
Data Analysis
Parental demographics were reported as frequencies with percentages and compared between groups using Fisher’s exact test. Cardiologist survey results were reported as mean scores with standard deviations and percentages of total observations. Comparison of survey results between the Model and Drawing groups was assessed using Kruskal–Wallis tests with median scores and first and third quartiles reported. Analyses were performed in R (version 4.2.0, The R Foundation, Vienna, Austria).
Results
Twenty-nine subjects were enrolled over a 12 month period. Eleven subjects were in the Drawing group and eighteen were in the Model group. The study cohort breakdown by group and diagnosis is shown in Fig. 3.
A summary of parental demographics in the Model and Drawing groups is shown in Table 1. Both the Model and Drawing groups had similar distributions in terms of age, race, household environment and income, education level and relationship status.
Results from the parental survey are summarized in Table 2. Parents in both groups scored well in the CHD knowledge section of the survey. A slightly higher, but not statistically significant improvement in parental knowledge was noted in the Model group (median score of 5 vs. 4, p = 0.23). Both groups scored similarly in self-reported understanding, self-reported confidence, helpfulness of the visualization tool, and improvement of communication experienced with the visualization tool. Lastly, the Model group had a lower median score on GAD-7 anxiety screening tool (3.5 vs. 6, p = 0.24) which is indicative of lower level of parental anxiety after consultation.
Eight fetal cardiology providers participated in the study. Results from the providers survey are summarized in Table 3. The cardiologists who counseled with the Model reported feeling satisfied with their consultation with a mean score of 8.9/10 and found the model useful to explain the CHD with a mean score of 8.7/10. A majority of them also felt that it improved their communication (83.3%). Two thirds of the cardiologists felt that it would be useful for parents to have models to take home with them (66.7%) and none felt that the model substantially lengthened the visit.
Discussion
Our study demonstrates that the routine use of 3DP cardiac models of CHD in fetal counseling sessions is feasible. The use of 3DP models to counsel families resulted in patient responses regarding knowledge and understanding which were not significantly different from current standard of care. In addition, although not found to be statistically significant with this number of participants, our data suggests that there were potential benefits for parents who were counseled with the 3DP model as they demonstrated higher knowledge-based scores and lower anxiety scale scores. Cardiologists did not report utilization of the models lengthened their visit compared to typical or average counseling sessions although this was a subjective measure and length of visit time was not measured quantitatively.
Our assessment of parental understanding was accomplished using two categories of questions. The first category consisted of knowledge-based questions about the CHD lesion with the expectant surgical management. The second category included subjective questions, allowing the parents to rate their own understanding, report on their confidence in ability to explain the CHD, and their attitude toward the visual aid used. Although not statistically significant potentially due to small sample size, parents in the model group did have slightly higher score in the first category of the parental assessment. Additionally, the Drawing group did have a higher proportion of parents with at least a college degree level of education although this demographic difference was not statistically significant and therefore unclear if impacted these results. A larger cohort would be useful to determine if these differences between the Model and Drawing groups are truly substantial.
The cardiologists’ assessment of parental understanding was well rated (mean score of 8.6/10) and for the majority of counseling sessions, the providers agreed that the model improved communication (83%) (Table 3). The “discrepancy” between the providers’ rating and the parental subjective rating of their own understanding (Table 2) could be due to the new exposure of learning the basics of CHD for the parents compared to the providers’ level of familiarity with CHD. It is possible that because the cardiologists were at a different level of baseline understanding, that they rated the additive value the models could provide differently. It would be interesting to evaluate the sequential use of 3DP models at follow-up counseling visits to assess if parental ratings of the benefit of the models changes over time.
Biglino et al. assessed the use of patient-specific 3DP cardiac models during outpatient cardiology consultation and found that the majority of parents reported the model to be useful during discussion with a cardiologist and rated the helpfulness of the 3DP model highly [15, 16]. These authors noted that many of the parents who participated in their study explicitly asked to keep the model. This was considered qualitative evidence that the models were well liked by families. In feedback provided by study participants, they reported that some of the traditional medical images and sketches were difficult to relate to. Cheuk et al. [26] surveyed parents of children with CHD in an outpatient clinic setting with a questionnaire that included components targeted at parental understanding of the nature and treatment of their child’s CHD. In this study, only 28.8% of their study cohort were able to correctly indicate their child’s heart lesion(s) diagrammatically. Awori et al. who examined the use of disease specific cardiac models in an outpatient setting found parents rated their understanding highest with physical 3DP models when compared to 2D drawings and 3D digital models [14]. Again, parents in this cohort were able to take the models home.
Models for this pilot study were all printed in a white thermoplastic. However, it would be interesting to explore multicolored models as they may result in more intuitive representations of the cardiac structures as well as oxygenated versus deoxygenated blood. These factors may impact overall parental understanding of the anatomy and hemodynamic impact of the CHD. It may also allow improved parental engagement with the model. The models used in our study were created from cardiac CT images. There is emerging literature related to the creation of 3D fetal cardiac models from spatiotemporal image correlation (STIC) volume-rendered echocardiogram data [27,28,29]. The potential of this technology could allow creation of patient and disease-specific fetal cardiac models increasing the potential for models which would better resemble individual cardiac anatomy.
Lastly, we sought to evaluate if there was any effect on counseling with a 3DP cardiac model on parental anxiety. There has been literature which demonstrated that a prenatal diagnosis of CHD is associated with inherent distress leading to parental stress [17,18,19] that can persist and result in greater postnatal anxiety [20,21,22]. The inherent distress from receiving a new prenatal diagnosis may hinder the exchange of knowledge during the prenatal visits. We theorized that the use of this educational tool may ease the emotional component of distress and anxiety inherent in receiving a prenatal diagnosis of CHD. The Model group did have an overall lower anxiety score categorized as minimal anxiety when compared to the drawing group whose scores were categorized as mild to moderate anxiety levels (median of 3.5 vs. 6). There were a greater proportion of patients with muscular ventricular septal defects in the Model group (10/18; 56% vs. the drawing group 3/11; 27%) which could potentially contribute to the lower anxiety scale scores seen in the Model group given the lower complexity of this lesion. The lack of statistical significance again may be due to the small cohort size. In addition, it may be helpful to utilize a pregnancy-specific scale as opposed to a generalized anxiety scale in order to have more tailored components to a population of expectant mothers.
Limitations of this pilot study include the small sample size, the evaluation of limited CHD lesions, and the partially subjective nature of the parental assessment tool used. Additionally, providers were asked to use a standardized drawing which may deviate from their typical practice. Many fetal cardiologists choose to draw the cardiac anatomy themselves. Therefore, the utilization of the standardized drawings may not accurately reflect the current practice for all fetal cardiology providers. The evaluation of a larger cohort could help better examine the trends seen in this pilot study. It may also allow for a meaningful sub-group analyses to better determine if certain populations or patient characteristics, such as education level, would benefit more from communication with a 3DP model. As a future step, it would be interesting to evaluate the use of a 3DP model in fetal counseling for more complex CHD lesions. For this pilot study, the use of simple, more common CHD lesions like VSD and coarctation of the aorta were chosen given that they are two of the lesions for which we most commonly counsel.
Conclusion
Use of a 3DP cardiac model during prenatal counseling is feasible and produces results related to parental understanding and knowledge that are at least similar to the current standard of care. This pilot study demonstrates routine use of 3DP models in fetal counseling were not detrimental to the transfer of information that occurs between fetal provider and parent and could even improve families’ learning and understanding of their child’s congenital heart lesion. Future directions include evaluation of a larger cohort and incorporation of models with more complex CHD which may increase the ability to detect the areas in which the models best facilitate fetal counseling.
Abbreviations
- CHD:
-
Congenital heart disease
- 3DP:
-
Three-dimensional printing
- 2D:
-
Two-dimensional
- VSD:
-
Ventricular septal defect
References
Bernier PL, Stefanescu A, Samoukovic G, Tchervenkov CI (2010) The challenge of congenital heart disease worldwide: epidemiologic and demographic facts. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 13(1):26–34
Atz AM, Travison TG, Williams IA et al (2010) Prenatal diagnosis and risk factors for preoperative death in neonates with single right ventricle and systemic outflow obstruction: screening data from the pediatric heart network single ventricle reconstruction trial∗. J Thorac Cardiovasc Surg 140(6):1245–1250
Illmann CF, Ghadiry-Tavi R, Hosking M, Harris KC (2020) Utility of 3D printed cardiac models in congenital heart disease: a scoping review. Heart 106:1631
Farooqi KM, Sengupta PP (2015) Echocardiography and three-dimensional printing: sound ideas to touch a heart. J Am Soc Echocardiogr 28(4):398–403
Farooqi KM, Nielsen JC, Uppu SC et al (2015) Use of 3-dimensional printing to demonstrate complex intracardiac relationships in double-outlet right ventricle for surgical planning. Circ Cardiovasc Imaging 8(5):e003043
Farooqi KM, Uppu SC, Nguyen K et al (2016) Application of virtual three-dimensional models for simultaneous visualization of intracardiac anatomic relationships in double outlet right ventricle. Pediatr Cardiol 37(1):90–98
Farooqi KM, Mahmood F (2018) Innovations in preoperative planning: insights into another dimension using 3D printing for cardiac disease. J Cardiothorac Vasc Anesth 32(4):1937–1945
Anwar S, Singh GK, Miller J et al (2018) 3D printing is a transformative technology in congenital heart disease. JACC Basic Transl Sci 3(2):294–312
Batteux C, Haidar MA, Bonnet D (2019) 3D-printed models for surgical planning in complex congenital heart diseases: a systematic review. Front Pediatr 7:23. https://doi.org/10.3389/fped.2019.00023
Smerling J, Marboe CC, Lefkowitch JH et al (2019) Utility of 3D printed cardiac models for medical student education in congenital heart disease: across a spectrum of disease severity. Pediatr Cardiol 40(6):1258–1265
Karsenty C, Guitarte A, Dulac Y et al (2021) The usefulness of 3D printed heart models for medical student education in congenital heart disease. BMC Med Educ 21(1):480
Loke YH, Harahsheh AS, Krieger A, Olivieri LJ (2017) Usage of 3D models of tetralogy of Fallot for medical education: impact on learning congenital heart disease. BMC Med Educ 17(1):54
Guo HC, Wang Y, Dai J, Ren CW, Li JH, Lai YQ (2018) Application of 3D printing in the surgical planning of hypertrophic obstructive cardiomyopathy and physician-patient communication: a preliminary study. J Thorac Dis 10(2):867–873
Awori J, Friedman SD, Chan T et al (2021) 3D models improve understanding of congenital heart disease. 3D Print Med. 7(1):26
Biglino G, Capelli C, Wray J et al (2015) 3D-manufactured patient-specific models of congenital heart defects for communication in clinical practice: feasibility and acceptability. BMJ Open 5(4):e007165–e007165
Biglino G, Koniordou D, Gasparini M et al (2017) Piloting the use of patient-specific cardiac models as a novel tool to facilitate communication during cinical consultations. Pediatr Cardiol 38(4):813–818
Rychik J, Donaghue DD, Levy S et al (2013) Maternal psychological stress after prenatal diagnosis of congenital heart disease. J Pediatr 162(2):302-307.e1
Bevilacqua F, Palatta S, Mirante N et al (2013) Birth of a child with congenital heart disease: emotional reactions of mothers and fathers according to time of diagnosis. J Matern Fetal Neonatal Med 26(12):1249–1253. https://doi.org/10.3109/14767058.2013.776536
Brosig CL, Whitstone BN, Frommelt MA, Frisbee SJ, Leuthner SR (2007) Psychological distress in parents of children with severe congenital heart disease: the impact of prenatal versus postnatal diagnosis. J Perinatol 27(11):687–692
Fonseca A, Nazaré B, Canavarro MC (2012) Parental psychological distress and quality of life after a prenatal or postnatal diagnosis of congenital anomaly: a controlled comparison study with parents of healthy infants. Disabil Health J 5(2):67–74
Skari H, Malt UF, Bjornland K et al (2006) Prenatal diagnosis of congenital malformations and parental psychological distress–a prospective longitudinal cohort study. Prenat Diagn 26(11):1001–1009
Bratt E-L, Järvholm S, Ekman-Joelsson B-M et al (2019) Parental reactions, distress, and sense of coherence after prenatal versus postnatal diagnosis of complex congenital heart disease. Cardiol Young 29(11):1328–1334
Farooqi KM, Lengua CG, Weinberg AD, Nielsen JC, Sanz J (2016) Blood pool segmentation results in superior virtual cardiac models than myocardial segmentation for 3D printing. Pediatr Cardiol 37(6):1028–1036
Cignoni P, Corsini M, Dellepiane M, Ganovelli F, Ranzuglia G (2008) MeshLab: an open-source mesh processing tool. Sixth eurographics Italian chapter conference. The Eurographics Association, Italy, pp 129–136
Spitzer RL, Kroenke K, Williams JBW, Löwe B (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166(10):1092
Cheuk DKL, Wong SMY, Choi YP, Chau AKT, Cheung YF (2004) Parents’ understanding of their child’s congenital heart disease. Heart 90(4):435–439
Huang J, Shi H, Chen Q et al (2021) Three-dimensional printed model fabrication and effectiveness evaluation in fetuses with congenital heart disease or with a normal heart. J Ultrasound Med 40(1):15–28
Veronese P, Bertelli F, Cattapan C, Andolfatto M, Gervasi MT, Vida VL (2020) Three-dimensional printing of the fetal heart with complete atrioventricular septal defect based on ultrasound data. Kardiol Pol 78(9):930–931
Veronese P, Bertelli F, Cattapan C, Andolfatto M, Gervasi MT, Vida VL (2021) Three-dimensional printing of fetal heart with d-transposition of the great arteries from ultrasound imaging data. World J Pediatr Congenit Heart Surg 12(2):291–292
Acknowledgements
This work was supported by a grant from Matthew’s Hearts of Hope and The Rachel Cooper Innovative Technologies Program.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Nicole Marella, Adriana Montes Gil, Weijia Fan, Chantal Angueyra Aristizabal, Priyanka Asrani, Jamie K. Harrington, Alexandra Channing, Matan Setton, Amee M. Shah, Stéphanie Levasseur, Julie Glickstein and Kanwal M. Farooqi. The first draft of the manuscript was written by Nicole Marella and Kanwal Farooqi and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any relevant financial or non-financial conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marella, N.T., Gil, A.M., Fan, W. et al. 3D-Printed Cardiac Models for Fetal Counseling: A Pilot Study and Novel Approach to Improve Communication. Pediatr Cardiol 44, 1800–1807 (2023). https://doi.org/10.1007/s00246-023-03177-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-023-03177-y