Abstract
Background
Mechanical ischemic preconditioning (MIPC) is defined as applying brief periods of ischemia before tissue reperfusion. This mechanism protects tissues against injury from sustained ischemia followed by reperfusion. We aimed to analyze the effects of MIPC on the tolerance of muscle flap tissue depending on the type and duration of ex vivo cold ischemia storage.
Methods
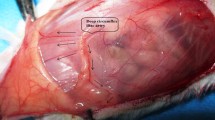
We studied the effects of MIPC on interstitial edema, inflammation, and muscle necrosis. Thirty-two porcine latissimus dorsi flaps were equally divided over four groups. Groups were divided based on the application of MIPC (every 15 min for a total of 1 h) or not, and the submersion into heparin or IGL-1®. Iterative biopsies were performed before harvesting the flap and one, two and 3 h after cold ischemia storage.
Results
Preconditioning free flaps before cold storage in heparin significantly decreased muscle necrosis, interstitial edema, and muscle cell size. Respectively, a decrease of 67%, 37% and 28% was seen in this group (p < 0.05). Preconditioning free flaps before cold storage in IGL-1® reduced necrosis by 26%, interstitial edema by 37% and muscle cell size by 33% (p < 0.05).
Conclusions
We found that MIPC significantly reduces interstitial edema, inflammation and necrosis and may increase the rate of successful revascularizations. However, studies assessing those tissular damage parameters after reperfusion of the flap need to be performed to assess more correctly inflammation and post-operative infections and to confirm the potential benefits of ICP.
Level of evidence: Not gradable




Similar content being viewed by others
References
Khouri RK, Cooley BC, Kunselman AR, Landis JR, Yeramian P, Ingram D, Natarajan N, Benes CO, Wallemark C (1998) A prospective study of microvascular free-flap surgery and outcome. Plast Reconstr Surg 102(3):711–721. https://doi.org/10.1097/00006534-199809030-00015
Bschorer R, Blake F, Lisboa B (1997) Free flap transfer and the prevention of endothelial damage. Mund-, Kiefer- und Gesichtschirurgie : MKG 1(4):235–238. https://doi.org/10.1007/BF03043556
Messner F, Grahammer J, Hautz T, Brandacher G, Schneeberger S (2016) Ischemia/reperfusion injury in vascularized tissue allotransplantation: tissue damage and clinical relevance. Curr Opin Organ Transplant 21(5):503–509. https://doi.org/10.1097/MOT.0000000000000343
Chen KT, Mardini S, Chuang DC, Lin CH, Cheng MH, Lin YT, Huang WC, Tsao CK, Wei FC (2007) Timing of presentation of the first signs of vascular compromise dictates the salvage outcome of free flap transfers. Plast Reconstr Surg 120(1):187–195. https://doi.org/10.1097/01.prs.0000264077.07779.50
Crawley MB, Sweeny L, Ravipati P, Heffelfinger R, Krein H, Luginbuhl A, Goldman R, Curry J (2019) Factors associated with free flap failures in head and neck reconstruction. Otolaryngol--Head Neck Surg: Off J Am Acad Otolaryngol-Head Neck Surg 161(4):598–604. https://doi.org/10.1177/0194599819860809
Biemer E (1981) Salvage operations for complication following replantation and free tissue transfer. Int Surg 66(1):37–38
Amin KR, Wong JKF, Fildes JE (2017) Strategies to reduce ischemia reperfusion injury in vascularized composite allotransplantation of the limb. J Hand Surg 42(12):1019–1024. https://doi.org/10.1016/j.jhsa.2017.09.013
Le Meur Y, Badet L, Essig M, Thierry A, Büchler M, Drouin S, Deruelle C, Morelon E, Pesteil F, Delpech PO, Boutin JM, Renard F, Barrou B (2020) First-in-human use of a marine oxygen carrier (M101) for organ preservation: a safety and proof-of-principle study. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg 20(6):1729–1738. https://doi.org/10.1111/ajt.15798
Figueroa BA, Said SA, Ordenana C, Rezaei M, Orfahli LM, Dubé GP, Papay F, Brunengraber H, Dasarathy S, Rampazzo A, Gharb BB (2022) Ex vivo normothermic preservation of amputated limbs with a hemoglobin-based oxygen carrier perfusate. J Trauma Acute Care surg 92(2):388–397. https://doi.org/10.1097/TA.0000000000003395
Burlage LC, Lellouch AG, Taveau CB, Tratnig-Frankl P, Pendexter CA, Randolph MA, Porte RJ, Lantieri LA, Tessier SN, Cetrulo CL Jr, Uygun K (2022) Optimization of ex vivo machine perfusion and transplantation of vascularized composite allografts. J Surg Res 270:151–161. https://doi.org/10.1016/j.jss.2021.09.005
Li DY, Shi XJ, Li W, Sun XD, Wang GY (2016) Ischemic preconditioning and remote ischemic preconditioning provide combined protective effect against ischemia/reperfusion injury. Life Sci 150:76–80. https://doi.org/10.1016/j.lfs.2016.02.077
Mounsey RA, Pang CY, Forrest C (1992) Preconditioning: a new technique for improved muscle flap survival. Otolaryngology--Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg 107(4):549–552. https://doi.org/10.1177/019459989210700406
Küntscher MV, Hartmann B, Germann G (2005) Remote ischemic preconditioning of flaps: a review. Microsurgery 25(4):346–352. https://doi.org/10.1002/micr.20123
Stokfisz K, Ledakowicz-Polak A, Zagorski M, Zielinska M (2017) Ischaemic preconditioning - current knowledge and potential future applications after 30 years of experience. Adv Med Sci 62(2):307–316. https://doi.org/10.1016/j.advms.2016.11.006
Rosenberg JH, Werner JH, Moulton MJ, Agrawal DK (2018) Current modalities and mechanisms underlying cardioprotection by ischemic conditioning. J Cardiovasc Transl Res 11(4):292–307. https://doi.org/10.1007/s12265-018-9813-1
Martou G, O’Blenes CA, Huang N, McAllister SE, Neligan PC, Ashrafpour H, Pang CY, Lipa JE (2006) Development of an in vitro model for study of the efficacy of ischemic preconditioning in human skeletal muscle against ischemia-reperfusion injury. J Appl Physiol (Bethesda, Md. : 1985) 101(5):1335–1342. https://doi.org/10.1152/japplphysiol.00278.2006
Moses MA, Addison PD, Neligan PC, Ashrafpour H, Huang N, McAllister SE, Lipa JE, Forrest CR, Pang CY (2005) Inducing late phase of infarct protection in skeletal muscle by remote preconditioning: efficacy and mechanism. Am J Physiol Regul Integr Comparative Physiol 289(6):R1609–R1617. https://doi.org/10.1152/ajpregu.00395.2005
Dragu A, Taeger CD, Buchholz R, Sommerfeld B, Hübner H, Birkholz T, Kleinmann JA, Münch F, Horch RE, Präbst K (2012) Online oxygen measurements in ex vivo perfused muscle tissue in a porcine model using dynamic quenching methods. Arch Orthop Trauma Surg 132(5):655–661. https://doi.org/10.1007/s00402-011-1458-3
Ghetu N, Mojallal A-A, Ghetu D, Iliescu V, Ilie V, Ilie V (2010) Endoscopic-assisted harvest of pedicled and free latissimus dorsi muscle in pigs. Timisoara Med J 145–53. https://www.researchgate.net/publication/287944163_Endoscopicassisted_harvest_of_pedicled_and_free_latissimus_dorsi_muscle_in_pigs
Yang M, Angel MF, Pang Y, Angel JJ, Wang Z, Neumeister MW, Wetter N, Zhang F (2012) Expression of inducible nitric oxide synthase in muscle flaps treated with ischemic postconditioning. Hand (New York, N.Y.) 7(3):297–302. https://doi.org/10.1007/s11552-012-9423-3
Wagh M, Pantazi G, Romeo R, Hurley JV, Morrison WA, Knight KR (2000) Cold storage of rat skeletal muscle free flaps and pre-ischemic perfusion with modified UW solution. Microsurgery 20(7):343–349. https://doi.org/10.1002/1098-2752(2000)20:7%3c343::aid-micr6%3e3.0.co;2-c
Kaufman T, Granick MS, Hurwitz DJ, Klain M (1987) Is experimental muscle flap temperature a reliable indicator of its viability? Ann Plast Surg 19(1):34–41. https://doi.org/10.1097/00000637-198707000-00005
Fowler JD, Li X, Cooley BC (1999) Brief ex vivo perfusion with heparinized and/or citrated whole blood enhances tolerance of free muscle flaps to prolonged ischemia. Microsurgery 19(3):135–140. https://doi.org/10.1002/(sici)1098-2752(1999)19:3%3c135::aid-micr3%3e3.0.co;2-y
Li X, Cooley BC, Gould JS (1993) Ex vivo perfusion with anticoagulated blood decreases ischemia/reperfusion injury. The Journal of hand surgery 18(4):629–634. https://doi.org/10.1016/0363-5023(93)90306-N
Werner NL, Alghanem F, Rakestraw SL, Sarver DC, Nicely B, Pietroski RE, Lange P, Rudich SM, Mendias CL, Rojas-Pena A, Magee JC, Bartlett RH, Ozer K (2017) Ex situ perfusion of human limb allografts for 24 hours. Transplantation 101(3):e68–e74. https://doi.org/10.1097/TP.0000000000001500
Couteau C, Rem K, Guillier D, Moris V, Revol M, Cristofari S (2018) Improving free-flap survival using intra-operative heparin: ritualistic practice or evidence-base medicine? A systematic review. Ann Chir Plast Esthet 63(3):e1–e5. https://doi.org/10.1016/j.anplas.2017.06.010
Fernández-Lázaro D, Díaz J, Caballero A, Córdova A (2019) The training of strength-resistance in hypoxia: effect on muscle hypertrophy. Entrenamiento de fuerza y resistencia en hipoxia: efecto en la hipertrofia muscular. Biomedica Revista del Instituto Nacional de Salud 39(1):212–220. https://doi.org/10.7705/biomedica.v39i1.4084
de Groot H, Rauen U (2007) Ischemia-reperfusion injury: processes in pathogenetic networks: a review. Transpl Proc 39(2):481–484. https://doi.org/10.1016/j.transproceed.2006.12.012
Harder Y, Amon M, Laschke MW, Schramm R, Rücker M, Wettstein R, Bastiaanse J, Frick A, Machens HG, Küntscher M, Germann G, Vollmar B, Erni D, Menger MD (2008) An old dream revitalised: preconditioning strategies to protect surgical flaps from critical ischaemia and ischaemia-reperfusion injury. J Plast Reconstruct Aesthet Surg: JPRAS 61(5):503–511. https://doi.org/10.1016/j.bjps.2007.11.032
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Sarra Cristofari, Sara Leuzzi and Alessio Stivala. The first draft of the manuscript was written by Sarra Cristofari and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the policies described in the Guide for the Care and Use of Laboratory Animals. Approval was granted by the Ethics Committee of the Sorbonne University (No. 16–001—APAFiS #9221).
Competing interests
Sarra Cristofari, Alessio Stivala, Sara Leuzzi, Loïc Van Dieren, Lorraine Litrico, Curtis L. Cetrulo Jr., Anne Janin, and Alexandre G. Lellouch declare no competing interests.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cristofari, S., Stivala, A., Leuzzi, S. et al. Use of mechanical preconditioning for free flaps in a swine model. Eur J Plast Surg 46, 645–652 (2023). https://doi.org/10.1007/s00238-023-02096-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02096-8