Abstract
Background
Various classifications of mandibular defects have been attempted, but no universally accepted system exists. After 25 years of experience, the senior author idealized a new mandibulectomy classification which could give a more detailed anatomical description leading to a more precise algorithm for reconstruction.
Methods
A new classification of mandibular defects is proposed: class I (anterior arch), class II (body), class III (ascending ramus), class IV (hemimandibulectomy), and class V (extended mandibulectomy). Each class is further subdivided into those that preserve or resect intra- and/or extraoral soft tissues (ABCD). This classification takes in account four factors that need to be thought when planning mandibular reconstruction: location/specificity of the defect, osteotomies, and bone and soft tissue requirements.
Results
A total of 218 defects were classified according to this new classification. Nearly 40% of the cases were classified as a class I defect followed by class IV (36,7%), class II (16%), class V (6,8%), and class III (0,5%). The authors also created an algorithm for reconstruction. In cases of an “only-bone” defect, the free iliac crest flap is the preferable choice, especially in class I and IV. When intra- or extraoral soft tissue is needed (types B and C), the fibula flap is our choice of excellence. In cases of extensive defects (type D), the fibula flap and the sequentially linked flow through flap are the preferred options.
Conclusions
Optimizing mandibular defect classification with better integration of data-driven information along with clinicopathological evidences and related experience allows for better clinical judgment and choices. We believe that our new classification system and algorithm for reconstruction can be a valuable guiding tool for dealing with complex mandibular reconstruction.
Level of evidence:
Level III, therapeutic study
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Classifications of mandibular defects have been attempted in the past. In Russian literature, Pavlov, in 1974, reviewed the case histories and roentgenograms of 215 patients and divided mandibular defects into 3 classes according to whether the remaining arch was left in one, two, or three fragments [1]. His classification highlighted the importance of the absence of two key elements in the mandibular arch: the condyle and the mentum. The importance of these two last bone landmarks was also the basis for the A to F David et al. classification (1988) [2], as well as for the HCL classifications, described by Jewer et al. (1989) [3] and Boyd et al. (1992) [4]. David’s classification has the following shortcomings: (1) no accounting for the soft tissue component and (2) certain mandibular defects are not represented which served primarily to describe their own patients. These shortcomings were partially solved by Jewer and Boyd’s classifications.
Nevertheless, Urken et al. (1991) [5] further highlighted these points, particularly the soft tissue component importance for reconstruction, which they concluded to be of equal or, sometimes greater impact, on the anatomofunctional end result when comparing with the bone defect present. In their retrospective study of 71 oromandibular reconstructions, they set forth a comprehensive classification of composite oromandibular defects, which included not only the bony and soft tissue components, but also neurologic defects. This classification was anatomically based and had 20 possibilities for bony defects, 22 for soft tissue defects, and 8 for neurologic deficits, which turned out to be impractical for clinical use. Regardless, it is to Urken et al. that we owe the concept of the reconstructive difficulty and, therefore, the functional and aesthetic outcomes, depending on more factors than just the size of the bony gap.
Takushima et al. (2001) [6], based on 178 cases, also suggested that the soft tissue defect is a critical factor for determining the appropriated flap for reconstruction. This point is the reason for our conceptual designation of lower face defects.
Recently, Schultz et al. (2014) [7], based on 24 patients, proposed a classification of mandible defects and a treatment algorithm, focusing on recipient vasculature and donor-free flap characteristics. Brown et al. (2016) [8] presented an interesting data analysis based on 49 from 167 studies of the scientific literature, which they considered to be sufficiently descriptive of the mandible defect for proper analysis. On the basis of these findings, a new classification is suggested based on the four corners of the mandible (two angles and two canines): class I, lateral; class II, hemimandibulectomy; class III, anterior; and class IV, extensive. They concluded three main points: (1) the increasing defect class relates to the size of the defect, osteotomy rate, and functional and aesthetic outcomes; (2) the development of an algorithm is tempting, but many confounding factors would make its use cumbersome; and (3) not incorporating the soft tissues defects in their classification constitutes a drawback.
Cordeiro et al., based on 202 patients with mandibulectomy defects [9], gave clinical background to Brown et al.’s last data analysis and their classification. In this paper, the authors described the importance of the soft tissue defects, location, and size and proposed a mandibulectomy classification and an algorithm for oromandibular reconstruction.
After 25 years dealing with head and neck reconstruction, the senior author (HC) of this article felt the need to idealize a new mandibulectomy classification which could give a more detailed anatomical defect description leading to a more precise algorithm of reconstruction, almost directed case to case. These experienced thoughts are based in 218 clinical cases.
Material and methods
This is a retrospective observational study that includes 218 cases submitted to segmental mandibular excision and immediate reconstruction with free flaps between 1996 and 2021.
Based on these clinical cases, their corresponding defects, and free flap reconstructions performed during the last 25 years by the senior author (HC), a classification system for mandibulectomy/lower face defects is proposed. Divided in five classes of defects, each one can be further subdivided in: A, only bone defect; B, intraoral soft tissue defect; C, extraoral soft tissue defect; and D, transmural defect (Fig. 1).
Class I defects (arch mandibulectomy) include segmental resections of the mandible arch, which can go until and reach the retromolar bone regions. This class of defects can be further subdivided into those that preserve or resect intra- and/or extraoral soft tissues (ABCD).
Mandibulectomy classification and algorithm proposed by the authors. Types: A, only bone defect; B, intraoral defect; C, extraoral defect; D, intra- and extraoral defect. OFC, osteofasciocutaneus; OM, osteomuscular; OMC, osteomusculocutaneus; OMFC, osteomusculofasciocutaneus; SLFTF, sequentially linked flow through flap
Class II defects (body mandibulectomy) include segmental resections of the mandibular body, between the canine dental unit and the retromolar bone regions. Class II defects can be further subdivided into those that preserve or resect intra- and/or extraoral soft tissues (ABCD).
Class III defects (ascending ramus mandibulectomy) include segmental resections of the ascending ramus until the retromolar bone regions. This class of defects can include or not the condyle (c). These defects can be further subdivided into those that preserve or resect intra- and/or extraoral soft tissues (ABCD).
Class IV defects (hemimandibulectomy) include segmental resections of the hemimandible until the midline. This class of defects can include or not the condyle (c). This class of defect can be further subdivided into those preserve or resect intra- and/or extraoral soft tissues (ABCD.
Class V defects (extended mandibulectomy) include segmental resection of the hemimandible beyond the midline. This class of defects can include or not the condyle (c). This class of defect can be further subdivided into those that preserve or resect intra- and/or extraoral soft tissues (ABCD).
Descriptive analysis of patient characteristics was carried out using SPSS software version 26.0 (IBM, Armonk, NY, USA).
This study followed the Declaration of Helsinki on medical protocol and ethics and was approved by the Hospital Ethical Commission number 39/2022.
Patients signed informed consent regarding the publishing of their data and photographs.
Results
In this cohort, 218 oromandibular defects corresponding to 225 reconstructive surgeries (7 patients were operated twice due to flap necrosis) were classified according to the authors’ proposed classification (Table 1).
Nearly 40% of the cases were classified as a class I defect (mandible arch), followed by class IV (hemimandibulectomy, 36,7%), class II (body, 16%), class V (extended hemimandibulectomy, 6,8%), and finally class III (ascending ramus, 0,5%).
In class I defects, it has been noticed that 46% of the defects had an intraoral tissue loss (type B) that needed to be reconstructed, and in 58% of them, OFC fibula was the flap used, but the myosseus fibula with the flexor hallux longus or the iliac crest with the internal oblique muscle flaps were also selected in some cases. The myosseus flaps were also used in class IIB and IVB (Table 1).
In class I, as an anterior arch defect, 1 or 2 osteotomies were needed in 87% of the cases. In cases classified as class II or III, no osteotomies were needed. Although one could think that class IV could be in line with class I, the use of the iliac crest flap with its specific curvature in 40 defects made possible that no osteotomies were performed in 63% of the cases.
All the defects with a through-and-through tissue loss (type D), whatever the location and because more skin was needed, were reconstructed with two possible options: an OFC fibula flap or a sequentially linked flow through flap.
The bone volume, the osteotomies design, and soft tissue requirements are three factors that need to be taking in account when planning the reconstruction. This classification allows the surgical team to think about these 3 factors when choosing the type and at the same time reduces the errors related to defect localization because of its specificity.
Based on these oromandibular defects, the authors created an algorithm for reconstruction (Fig. 1). In cases of an “only bone defect,” the OM iliac crest is the preferable choice especially in class I and IV (Fig. 2). When intra- or extraoral soft tissue is needed (types B and C), the OFC fibula is our choice of excellence, usually associated with osteotomies in class I, IV, and V (Fig. 3). In cases of extensive defect including intra- and extraoral soft tissue (Type D), the OFC fibula flap and the sequentially linked flow through flap are the options (Fig. 4).
a–d Male, 46 years old, with a status post excision of a squamous cell carcinoma with a defect from the right ascending ramus (subcondyle) until 3.5. The osseous reconstruction was performed with an iliac myosseous flap with an osteotomy. The postoperative picture shows the contour obtained. This patient has a perceptible speech with no oral rehabilitation (mandibulectomy type VA preserving condyle)
a–d Male, 39 years old, presented with a squamous cell carcinoma of the floor of the mouth, with a resection defect that included the mandible arch from 4.8 until 3.8, floor of the mouth and 1/3 of the anterior tongue. In this case, the OFC fibula flap was selected with an intraoral skin coverage. This patient has a perceptible speech. The postoperative picture shows the aesthetic result with no oral rehabilitation preformed (mandibulectomy type IB)
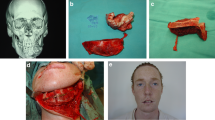
a–e Male, 59 years old, recurrent basocellular carcinoma of the chin invading the mandible and floor of the mouth. The mandible defect was angle to angle including an intra- and extraoral soft tissue defect which corresponds to a mandibulectomy type ID in the authors classification. It was reconstructed using the sequentially link flow through flap concept with an OFC fibula flap (intraoral skin and 2 osteostomies) and FC radial forearm flap (extraoral skin) (mandibulectomy type ID)
The OFC radial forearm flap was used by the authors in the beginning of this series as an option for bone stock and skin coverage. This flap was overtaken by fibula and iliac crest. The radial forearm flap is still used as a soft tissue donor in the sequentially linked flow through flap concept and when the other flaps are not available for harvesting.
Discussion
The major aims of a classification system are the relation between functional and aesthetic complexity of the oromandibular defects and the provision of a framework for a reconstructive algorithm. Consequently, another main purpose is reached by this double achievement—allowance of a common language for meaningful scientific interchange between the various schools of knowledge.
We agree with Brown et al. [8] that still no universally accepted classification system exists for mandibular defects. An important drawback exists inside their classification, which is the lack of the incorporation of soft tissue defects. Although their theoretical classification is logical and simple, the regional mandible anatomy is more complex than just four corners. Also, we fully disagree with two of their statements: (1) “For a classification to be adopted, simplicity and logic are paramount and we can see no effective method to incorporate further elements to describe this oncological defect.” (2) “Although the development of an algorithm is tempting, because it could help decide the most appropriate reconstruction for the mandibular defect, many confounding factors would make use of this algorithm cumbersome.”
Also, it is not our understanding Cordeiro’s et al. [9] conclusive point, which states that as the extent of the soft tissue defect increases, non-osseous flaps are preferred due to greater reliability of skin island. In such large compound resections, the sequentially linked flow-through flap concept should be selected and applied with very interesting results [10]. This being stated, we fully agree with these last authors that sometimes the soft tissue reconstructive needs supersede the bony needs.
Our algorithm points that when the mandibular defect is only bone, the myosseous iliac crest flap is the first choice leading to better aesthetic and oral rehabilitation outcomes. When the soft tissue component intra- or extraoral enlarges, the osteocutaneus fibula flap is the paramount flap either intraoral (B), extraoral (C), or through and through (D) defects. Osteomyocutaneus iliac crest flap is a reconstructive option which must not be forgotten in type IC defects where the thick soft tissue component of this great flap allows a good contour.
If the ladder of oncological or osteoradionecrosis resections and trauma defects rises for very extensive defects, our experience says that the sequentially linked flow through flap concept is the option.
In the last decades, evolution in reconstructive surgery has put the standard of care in a higher level. The treatment goal of restoring function as the first priority has been caught up by a new goal—the aesthetic result. Therefore, we should seek for facial harmony and symmetry. Our classification of mandibulectomy defects and reconstruction algorithm stands on these clinicopathological evidences and related experience.
Our algorithm clearly points that when the mandible defect is only bone, myosseus iliac crest flap is the first choice regarding the end results on aesthetic and oral rehabilitation quality.
Unsolved problems still remain, which leave an open path for future advances. Gaia’s plastic reconstructive craniomaxillofacial hand and microsurgical unit is trying hard to contribute for other advances to come. Always consider the hard as well as the soft tissues of the lower face when dealing with oromandibular reconstruction.
References
Pavlov BL (1974) Classification of mandibular defects. Stomatologiia (Mosk) 53(5):43–46
David DJ et al (1988) Mandibular reconstruction with vascularized iliac crest: a 10-year experience. Plast Reconstr Surg 82(5):792–803
Jewer DD et al (1989) Orofacial and mandibular reconstruction with the iliac crest free flap: a review of 60 cases and a new method of classification. Plast Reconstr Surg 84(3):391–403 (discussion 404-5)
Boyd JB et al (1993) Classification of mandibular defects. Plast Reconstr Surg 92(7):1266–1275
Urken ML et al (1991) Oromandibular reconstruction using microvascular composite free flaps. Report of 71 cases and a new classification scheme for bony, soft-tissue, and neurologic defects. Arch Otolaryngol Head Neck Surg 117(7):733–44
Takushima A et al (2001) Mandibular reconstruction using microvascular free flaps: a statistical analysis of 178 cases. Plast Reconstr Surg 108(6):1555–1563
Schultz BD et al (2015) Classification of mandible defects and algorithm for microvascular reconstruction. Plast Reconstr Surg 135(4):743e–754e
Brown JS et al (2016) A new classification for mandibular defects after oncological resection. Lancet Oncol 17(1):e23-30
Cordeiro PG, Henderson PW, Matros E (2018) A 20-year experience with 202 segmental mandibulectomy defects: a defect classification system, algorithm for flap selection, and surgical outcomes. Plast Reconstr Surg 141(4):571e–581e
Costa H et al (2012) Flow-through sequentially linked free flaps in head and neck reconstruction. Eur J Plast Surg 35(1):31–41
Acknowledgements
The authors would like to thank Susana Ferreira, unit secretary, for her help, support, and typing of this paper. Their thanks also go to the architect Maria Pais de Sousa for the drawings.
Funding
Open access funding provided by FCT|FCCN (b-on).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
This study followed the Declaration of Helsinki on medical protocol and ethics and was approved by the Centro Hospitalar Vila Nova de Gaia/Espinho Ethical Board – number 39/2022.
Patient consent
Informed consent was obtained by the patients for the use of their data and images.
Conflict of interest
Horácio Zenha, Marta Sá de Azevedo, Rui Vieira, and Horácio Costa declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zenha, H., Azevedo, M., Vieira, R. et al. Microsurgical reconstruction of the mandible part II: new classification system and algorithm. Eur J Plast Surg 46, 707–716 (2023). https://doi.org/10.1007/s00238-023-02072-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02072-2