Abstract
Purpose
The aim of this study was to explore patterns and long-term development in prescribing potentially inappropriate medication (PIM) according to the EU(7)-PIM list to elderly patients in Germany.
Methods
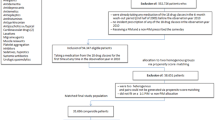
We analysed anonymized German claims data. The study population comprised 6.0 million insured individuals at least 65 years old, including all their prescriptions reimbursed in 2019. For the analysis of long-term development, we used data for the years 2009–2019. Factors associated with PIM prescribing were considered from two perspectives: patient-oriented analysis was performed with logistic regression and prescriber-oriented analysis was performed with multiple linear regression.
Results
EU(7)-PIM prevalence was reduced from 56.9% in 2009 to 45.1% in 2019. Average annual volume (DDDs/insured) decreased from 145 in 2009 to 121 in 2019. These figures are substantially greater than those for the older PRISCUS list. The majority of investigated ATC level 2 groups with the highest EU(7)-PIM DDD volume exhibited substantial decreases; moderate increases were found for antihypertensive and urological drugs. Antithrombotics increased strongly with the introduction of direct oral anticoagulants. The most prevalent EU(7)-PIM medication was diclofenac; however, in the age group 85+ years, apixaban was twice as prevalent as diclofenac. Polypharmacy, female sex, age < 90 years, need for nursing care and living in Eastern regions were identified as risk factors. Prescriber specialty was the most marked factor in the prescriber-oriented analysis.
Conclusion
Although the use of EU(7)-PIMs has been declining, regional differences indicate considerable room for improvement. The comparison with PRISCUS highlights the necessity of regular updates of PIM lists.



Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available from Wissenschaftliches Institut der AOK (WIdO), Berlin, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of WIdO within the restrictions set out by the European General Data Protection Regulation (GDPR).
Code availability
Code is available from the authors (GWS, ISK) upon reasonable request.
References
Statistisches Bundesamt (Destatis) (2019) Bevölkerungspyramide: Altersstruktur Deutschlands von 1950 - 2060. https://service.destatis.de/bevoelkerungspyramide/index.html#!y=2029&a=20,65&l=en&g. Accessed 24 Nov 2020
Schmiedl S, Rottenkolber M, Szymanski J et al (2018) Preventable ADRs leading to hospitalization - results of a long-term prospective safety study with 6,427 ADR cases focusing on elderly patients. Expert Opin Drug Saf 17:125–137. https://doi.org/10.1080/14740338.2018.1415322
Bates DW, Cullen DJ, Laird N et al (1995) Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group JAMA 274:29–34
Morimoto T, Gandhi TK, Seger AC et al (2004) Adverse drug events and medication errors: detection and classification methods. Qual Saf Health Care 13:306–314. https://doi.org/10.1136/qhc.13.4.306
Reeve E, Wiese MD, Mangoni AA (2015) Alterations in drug disposition in older adults. Expert Opin Drug Metab Toxicol 11:491–508. https://doi.org/10.1517/17425255.2015.1004310
Thürmann PA (2020) Clinical studies in geriatric population. Drug Discov Eval Methods Clin Pharmacol 417–424. https://doi.org/10.1007/978-3-319-68864-0_43
Gallagher P, Barry P, O’Mahony D (2007) Inappropriate prescribing in the elderly. J Clin Pharm Ther 32:113–121. https://doi.org/10.1111/j.1365-2710.2007.00793.x
Beers MH, Ouslander JG, Rollingher I et al (1991) Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA Division of Geriatric Medicine. Arch Intern Med 151:1825–1832
Motter FR, Fritzen JS, Hilmer SN et al (2018) Potentially inappropriate medication in the elderly: a systematic review of validated explicit criteria. Eur J Clin Pharmacol 74:679–700. https://doi.org/10.1007/s00228-018-2446-0
Fialová D, Brkić J, Laffon B et al (2019) Applicability of EU(7)-PIM criteria in cross-national studies in European countries. Ther Adv Drug Saf 10:2042098619854014. https://doi.org/10.1177/2042098619854014
Wamil N, Mattsson S, Gustafsson M (2019) Assessment of potentially inappropriate medications using the EU (7)-PIM list and the Swedish quality indicators. Int J Clin Pharm 41:903–912. https://doi.org/10.1007/s11096-019-00847-x
Grina D, Briedis V (2017) The use of potentially inappropriate medications among the Lithuanian elderly according to Beers and EU(7)-PIM list - a nationwide cross-sectional study on reimbursement claims data. J Clin Pharm Ther 42:195–200. https://doi.org/10.1111/jcpt.12494
Toepfer S, Bolbrinker J, König M et al (2019) Potentially inappropriate medication in older participants of the Berlin Aging Study II (BASE-II) - sex differences and associations with morbidity and medication use. PLoS One 14:e0226511. https://doi.org/10.1371/journal.pone.0226511
Holt S, Schmiedl S, Thürmann PA (2010) Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arzteblatt Int 107:543–551. https://doi.org/10.3238/arztebl.2010.0543
Beers MH (1997) Explicit criteria for determining potentially inappropriate medication use by the elderly. An update Arch Intern Med 157:1531–1536
Fick DM, Cooper JW, Wade WE et al (2003) Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med 163:2716–2724. https://doi.org/10.1001/archinte.163.22.2716
McLeod PJ, Huang AR, Tamblyn RM, Gayton DC (1997) Defining inappropriate practices in prescribing for elderly people: a national consensus panel. CMAJ 156:385–391
Laroche M-L, Charmes J-P, Merle L (2007) Potentially inappropriate medications in the elderly: a French consensus panel list. Eur J Clin Pharmacol 63:725–731. https://doi.org/10.1007/s00228-007-0324-2
Renom-Guiteras A, Meyer G, Thürmann PA (2015) The EU(7)-PIM list: a list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur J Clin Pharmacol 71:861–875. https://doi.org/10.1007/s00228-015-1860-9
Bundesministerium der Justiz und für Verbraucherschutz (2020) Sozialgesetzbuch - Elftes Buch, § 15. https://www.gesetze-im-internet.de/sgb_11/__15.html. Accessed 24 Nov 2020
Gnjidic D, Tinetti M, Allore HG (2017) Assessing medication burden and polypharmacy: finding the perfect measure. Expert Rev Clin Pharmacol 10:345–347. https://doi.org/10.1080/17512433.2017.1301206
Nishtala PS, Salahudeen MS (2015) Temporal trends in polypharmacy and hyperpolypharmacy in older New Zealanders over a 9-year period: 2005–2013. Gerontology 61:195–202. https://doi.org/10.1159/000368191
Statistisches Bundesamt (Destatis) (2020) - GENESIS-Online. https://www-genesis.destatis.de/genesis/online. Accessed 24 Nov 2020
Monteiro C, Canário C, Ribeiro MÂ et al (2020) Medication evaluation in Portuguese elderly patients according to beers, STOPP/START criteria and EU(7)-PIM List - an exploratory study. Patient Prefer Adherence 14:795–802. https://doi.org/10.2147/PPA.S247013
Caldeira D, Nunes-Ferreira A, Rodrigues R et al (2019) Non-vitamin K antagonist oral anticoagulants in elderly patients with atrial fibrillation: a systematic review with meta-analysis and trial sequential analysis. Arch Gerontol Geriatr 81:209–214. https://doi.org/10.1016/j.archger.2018.12.013
Moudallel S, Steurbaut S, Cornu P, Dupont A (2018) Appropriateness of DOAC prescribing before and during hospital admission and analysis of determinants for inappropriate prescribing. Front Pharmacol 9:1220. https://doi.org/10.3389/fphar.2018.01220
American Geriatrics Society Beers Criteria® Update Expert Panel (2019) American Geriatrics Society 2019 Updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc 67:674–694. https://doi.org/10.1111/jgs.15767
Mucalo I, Hadžiabdić MO, Brajković A et al (2017) Potentially inappropriate medicines in elderly hospitalised patients according to the EU(7)-PIM list, STOPP version 2 criteria and comprehensive protocol. Eur J Clin Pharmacol 73:991–999. https://doi.org/10.1007/s00228-017-2246-y
Schubert I, Küpper-Nybelen J, Ihle P, Thürmann P (2013) Prescribing potentially inappropriate medication (PIM) in Germany’s elderly as indicated by the PRISCUS list. An analysis based on regional claims data. Pharmacoepidemiol Drug Saf 22:719–727. https://doi.org/10.1002/pds.3429
Stock S, Redaelli M, Simic D et al (2014) Risk factors for the prescription of potentially inappropriate medication (PIM) in the elderly: an analysis of sickness fund routine claims data from Germany. Wien Klin Wochenschr 126:604–612. https://doi.org/10.1007/s00508-014-0589-2
Roux B, Sirois C, Simard M et al (2020) Potentially inappropriate medications in older adults: a population-based cohort study. Fam Pract 37:173–179. https://doi.org/10.1093/fampra/cmz060
Sönnerstam E, Sjölander M, Gustafsson M (2017) An evaluation of the prevalence of potentially inappropriate medications in older people with cognitive impairment living in Northern Sweden using the EU(7)-PIM list. Eur J Clin Pharmacol 73:735–742. https://doi.org/10.1007/s00228-017-2218-2
Nothelle SK, Sharma R, Oakes A et al (2019) Factors associated with potentially inappropriate medication use in community-dwelling older adults in the United States: a systematic review. Int J Pharm Pract 27:408–423. https://doi.org/10.1111/ijpp.12541
Johnell K (2015) Inappropriate drug use in people with cognitive impairment and dementia: a systematic review. Curr Clin Pharmacol 10:178–184. https://doi.org/10.2174/1574884710666150609154741
Thürmann PA (2017) Einsatz von Psychopharmaka bei Pflegebedürftigen. In: Jacobs K, Kuhlmey A, Greß S, Klauber J, Schwinger A (eds) Pflege-Report 2017. Schattauer, Stuttgart, pp 119–129
Hoffmann F, Bantel C, von Rosen FT, Jobski K (2020) Regional differences in prescribing patterns of metamizole in Germany based on data from 70 million persons. Int J Environ Res Public Health 17:3892. https://doi.org/10.3390/ijerph17113892
Selke Krulichová I, Selke GW, Eichler U et al (2019) Impact of EU risk assessment process and administrative regulations for manufacturers of combined hormonal contraceptive prescribing. An analysis of developments in Germany and the implications. Curr Med Res Opin 35:697–704. https://doi.org/10.1080/03007995.2018.1541317
Gudd K, Meier F, Lindenthal J et al (2020) Potenziell inadäquate Medikation in einem deutschen Praxisnetz – Wer verordnet was an wen? Z Gerontol Geriat 53:647–654. https://doi.org/10.1007/s00391-019-01660-x
Funding
This project was financially supported by PROGRES Q40-09, a programme administered by Charles University, Prague.
Author information
Authors and Affiliations
Contributions
I. Selke Krulichová (ISK) and G. W. Selke (GWS) conceptualized the study with support from P.A. Thürmann (PAT). GWS analysed the data. ISK drafted the manuscript with support from GWS and PAT. All authors participated in critical revision of the manuscript, contributed comments and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Selke Krulichová, I., Selke, G.W. & Thürmann, P.A. Trends and patterns in EU(7)-PIM prescribing to elderly patients in Germany. Eur J Clin Pharmacol 77, 1553–1561 (2021). https://doi.org/10.1007/s00228-021-03148-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-021-03148-3