Abstract
Rationale
Depression in schizophrenia is an important symptom. We investigated whether depression and suicidal symptoms in the chronic phase are related to remote future clinical outcomes in patients with schizophrenia and whether psychotropics improved clinical outcomes.
Objectives
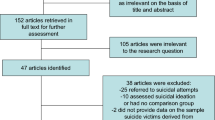
The subjects included 462 outpatients of working age (15 to 64 years old) with schizophrenia treated at Okayama University Hospital from January 2010 to December 2011. We investigated the relationship between the Clinical Global Impression-Severity score at the last visit (average 19.2 years) and the existence of previous depression, suicidal ideas, and suicide attempts. We adjusted by several possible confounders including medical history using multiple regression analysis or logistic regression analysis.
Results
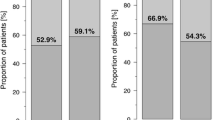
Of 462 patients, 168 (36.4%) presented with depression 2 years after schizophrenia onset. A history of suicidal ideas and attempts was related to worse clinical outcome. In males, a history of depression was related to worse clinical outcome, but not in females. Lithium carbonate was related to better clinical outcome in all schizophrenia patients with depression, especially in males. Treatment with antidepressants was related to better clinical outcome only in males.
Conclusions
A history of depression or suicidal symptoms in the chronic phase predicted the future worse clinical outcome in patients with schizophrenia. The administration of lithium carbonate or antidepressants might be recommended, especially to male schizophrenia patients with depression.
Similar content being viewed by others
References
Addington DE, Mohamed S, Rosenheck R, Davis SM, Stroup TS, McEvoy JP, Swartz MS, Lieberman JA (2011) Impact of second-generation antipsychotics and perphenazine on depressive symptoms in a randomized trial of treatment for chronic schizophrenia. J Clin Psychiatry 72:75–80
Bartko G, Herczeg I, Bekesy M (1987) Predicting outcome of neuroleptic treatment on the basis of subjective response and early clinical improvement. J Clin Psychiatry 48:363–365
Bauer M, Glenn T, Pilhatsch M, Pfennig A, Whybrow PC (2013) Gender differences in thyroid system function: relevance to bipolar disorder and its treatment. Bipolar Disord 16:58–71
Buckley PF, Miller BJ, Lehrer DS, Castle DJ (2009) Psychiatric comorbidities and schizophrenia. Schizophr Bull 35:383–402
Busner J, Targum SD (2007) The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (edgmont) 4:28–37
Clemmensen L, Vernal DL, Steinhausen HC (2012) A systematic review of the long-term outcome of early onset schizophrenia. BMC Psychiatry 12:150
Cohen LJ, Test MA, Brown RL (1990) Suicide and schizophrenia: data from a prospective community treatment study. Am J Psychiatry 147:602–607
Conley RR, Ascher-Svanum H, Zhu B, Faries DE, Kinon BJ (2007) The burden of depressive symptoms in the long-term treatment of patients with schizophrenia. Schizophr Res 90:186–197
Delahanty J, Ram R, Postrado L, Balis T, Green-Paden L, Dixon L (2001) Differences in rates of depression in schizophrenia by race. Schizophr Bull 27:29–38
Griffiths JJ, Zarate CA Jr, Rasimas JJ (2014) Existing and novel biological therapeutics in suicide prevention. Am J Prev Med 47:S195-203
Hafner H, Maurer K, Trendler G, Schmidt M, Könnecke R (2005) Schizophrenia and depression: challenging the paradigm of two separate diseases–a controlled study of schizophrenia, depression and healthy controls. Schizophr Res 77:11–24
Hasan A, Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF, Thibaut F, Möller H (2015) World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia. Part 3: Update 2015 Management of special circumstances: depression, suicidality, substance use disorders and pregnancy and lactation. World J Biol Psychiatry 16:142–170
Hawton K, Sutton L, Haw C, Sinclair J, Deeks JJ (2005) Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry 187:9–20
Hirsch SR, Jolley AG (1989) The dysphoric syndrome in schizophrenia and its implications for relapse. Br J Psychiatry Suppl 5:46–50
Hogarty GE, McEvoy JP, Ulrich RF, DiBarry AL, Bartone P, Cooley S, Hammill K, Carter M, Munetz MR, Perel J (1995) Pharmacotherapy of impaired affect in recovering schizophrenic patients. Arch Gen Psychiatry 52:29
Hor K, Taylor M (2010) Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol 24:81–90
Inada T, Inagaki A (2015) Psychotropic dose equivalence in Japan. Psychiatry Clin Neurosci 69:440–447
Johnson DA (1988) The significance of depression in the prediction of relapse in chronic schizophrenia. Br J Psychiatry 152:320–323
Käkelä J, Panula J, Oinas E, Hirvonen N, Jääskeläinen E, Miettunen J (2014) Family history of psychosis and social, occupational and global outcome in schizophrenia: a meta-analysis. Acta Psychiatr Scand 130:269–278
Kay SR, Lindenmayer JP (1987) Outcome predictors in acute schizophrenia. Prospective significance of background and clinical dimensions. J Nerv Ment Dis 175:152–160
Lang FU, Kösters M, Lang S, Becker T, Jäger M (2013) Psychopathological long-term outcome of schizophrenia – a review. Acta Psychiatr Scand 127:173–182
Lauronen E, Miettunen J, Veijola J, Karhu M, Jones PB, Isohanni M (2007) Outcome and its predictors in schizophrenia within the Northern Finland 1966 Birth Cohort. Eur Psychiatry 22:129–136
LeGates TA, Kvarta MD, Thompson SM (2019) Sex differences in antidepressant efficacy. Neuropsychopharmacol 44:140–154
Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, Kreyenbuhl J (2004) Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry 161:1–56
Leucht S, Kissling W, McGrath J (2004) Lithium for schizophrenia revisited: a systematic review and meta-analysis of randomized controlled trials. J Clin Psychiatry 65:177–186
Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM (2009) Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet 373:31–41
Leucht S, Heres S, Kissling W, Davis JM (2013) Pharmacological treatment of schizophrenia. Fortschr Neurol Psychiatr 81:e1-13
Mizrahi R, Rusjan P, Agid O, Graff A, Mamo DC, Zipursky RB, Kapur S (2007) Adverse subjective experience with antipsychotics and its relationship to striatal and extrastriatal D2 receptors: a PET study in schizophrenia. Am J Psychiatry 164:630–637
Moazen-Zadeh E, Bayanati S, Ziafat K, Rezaei F, Mesgarpour B, Akhondzadeh S (2020) Vortioxetine as adjunctive therapy to risperidone for treatment of patients with chronic schizophrenia: a randomised, double-blind, placebo-controlled clinical trial. J Psychopharmacol 34:506–513
Murray RM, Van Os J (1998) Predictors of outcome in schizophrenia. J Clin Psychopharmacol 18:2S-4S
Murru A, Carpiniello B (2018) Duration of untreated illness as a key to early intervention in schizophrenia: a review. Neurosci Lett 669:59–67
Newton R, Rouleau A, Nylander AG, Loze JY, Resemann HK, Steeves S, Crespo-Facorro B (2018) Diverse definitions of the early course of schizophrenia–a targeted literature review. NPJ Schizophr 4:21
Oakley P, Kisely S, Baxter A, Harris M, Desoe J, Dziouba A, Siskind D (2018) Increased mortality among people with schizophrenia and other non-affective psychotic disorders in the community: a systematic review and meta-analysis. J Psychiatr Res 102:245–253
Oosthuizen P, Emsley RA, Roberts MC, Turner J, Keyter L, Keyter N, Torreman M (2002) Depressive symptoms at baseline predict fewer negative symptoms at follow-up in patients with first-episode schizophrenia. Schizophr Res 8:247–252
Palmer BA, Pankratz VS, Bostwick JM (2005) The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry 62:247–253
Riedel M, Mayr A, Seemüller F, Maier W, Klingberg S, Heuser I, Klosterkötter J, Gastpar M, Schmitt A, Sauer H, Schneider F, Gaebel W, Jäger M, Möller HJ, Schennach-Wolff R (2012) Depressive symptoms and their association with acute treatment outcome in first-episode schizophrenia patients: comparing treatment with risperidone and haloperidol. World J Biol Psychiatry 13:30–38
Rubinow DR, Schmidt PJ (2019) Sex differences and the neurobiology of affective disorders. Neuropsychopharmacol 44:111–128
Rybakowski JK, Vansteelandt K, Szafranski T, Thys E, Jarema M, Fleischhacker WW, Kahn RS, Peuskens J (2012) Treatment of depression in first episode of schizophrenia: results from EUFEST. Eur Neuropsychopharmacol 22:875–882
Sakamoto S, Takaki M, Okahisa Y, Mizuki Y, Inagaki M, Ujike H, Mitsuhashi T, Takao S, Ikeda M, Uchitomi Y, Iwata N, Yamada N (2016) Individual risk alleles of susceptibility to schizophrenia are associated with poor clinical and social outcomes. J Hum Genet 61:329–334
Schennach-Wolff R, Obermeier M, Seemüller F, Jäger M, Messer T, Laux G, Pfeiffer H, Naber D, Schmidt LG, Gaebel W, Klosterkötter J, Heuser I, Maier W, Lemke MR, Rüther E, Klingberg S, Gastpar M, Möller HJ, Riedel M (2011) Evaluating depressive symptoms and their impact on outcome in schizophrenia applying the Calgary Depression Scale. Acta Psychiatr Scand 123:228–238
Siris SG, Addington D, Azorin JM, Falloon IR, Gerlach J, Hirsch SR (2001) Depression in schizophrenia: recognition and management in the USA. Schizophr Res 47:185–197
Strauss GP, Sandt AR, Catalano LT, Allen DN (2012) Negative symptoms and depression predict lower psychological well-being in individuals with schizophrenia. Compr Psychiatry 53:1137–1144
Suttajit S, Pilakanta S (2013) Prevalence of metabolic syndrome and its association with depression in patients with schizophrenia. Neuropsychiatr Dis Treat 9:941–946
Terao T, Oga T, Nozaki S, Ohta A, Ohtsubo Y, Yamamoto S, Zamami M, Okada M (1995) Lithium addition to neuroleptic treatment in chronic schizophrenia: a randomized, double-blind, placebo-controlled, cross-over study. Acta Psychiatr Scand 92:220–224
Terevnikov V, Stenberg JH, Tiihonen J, Joffe M, Burkin M, Tchoukhine E, Joffe G (2011) Add-on mirtazapine improves depressive symptoms in schizophrenia: a double-blind randomized placebo-controlled study with an open-label extension phase. Hum Psychopharmacol 26:188–193
Tomotake M, Kaneda Y, Iga J, Kinouchi S, Tayoshi S, Motoki I, Sumitani S, Yamauchi K, Taniguchi T, Ishimoto Y, Ueno S, Ohmori T (2006) Subjective and objective measures of quality of life have different predictors for people with schizophrenia. Psychol Rep 99:477–487
Voruganti L, Awad AG (2004) Neuroleptic dysphoria: towards a new synthesis. Psychopharmacol 171:121–132
Whitehead C, Moss S, Cardno A, Lewis G (2003) Antidepressants for the treatment of depression in people with schizophrenia: a systematic review. Psychol Med 33:589–599
Yada Y, Kitagawa K, Sakamoto S, Ozawa A, Nakada A, Kashiwagi H, Okahisa Y, Takao S, Takaki M, Kishi Y, Yamada N (2021) The relationship between plasma clozapine concentration and clinical outcome: a cross-sectional study. Acta Psychiatr Scand 143:227–237
Acknowledgements
The authors would like to thank the Zikei Institute of Psychiatry (Okayama, Japan).
Funding
This work was supported in part by an award from the Dopamine Partial Agonist Society (Tokyo, Japan) (Manabu Takaki).
Author information
Authors and Affiliations
Contributions
Y. Yamada, M. Takaki, M. Fujiwara, S. Sakamoto, Y. Okahisa, and N. Yamada participated in the design of the study, supervised the project, and contributed intellectually to the interpretation of the data. M. Takaki and S. Sakamoto investigated patient clinical records. Y. Yamauchi and S. Takao interpreted the statistical analyses. M. Takaki, M. Fujiwara, and S. Sakamoto revised critically. All authors contributed to and have approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
N.Y. has received unrestricted research funding from Daiichi Sankyo, Eisai, Pfizer, Otsuka, Astellas, and Merck Sharp & Dohme, which was deposited into research accounts at Okayama University. N.Y. has received honoraria for his participation as a speaker at educational events from UCB Japan, Tsumura, Pfizer, Dainippon-Sumitomo, Daiichi-Sankyo, Merck Sharp & Dohme, Pfizer, Eisai, Meiji-Seika, and Mochida.
M.T. has received honoraria for his participation as a speaker at educational events sponsored by Otsuka, Dainippon Sumitomo, and Takeda.
S.S. has received unrestricted research funding from Eli Lilly, which was deposited into research accounts at Okayama University Hospital. S.S. has received honoraria for his participation as a speaker at an educational event sponsored by Otsuka.
Y. Yamada, Y. Yamauchi, M.F., Y.O., and S.T. report no additional financial or other relationship relevant to this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yamada, Y., Yamauchi, Y., Sakamoto, S. et al. Association between depression in chronic phase and future clinical outcome of patients with schizophrenia. Psychopharmacology 239, 965–975 (2022). https://doi.org/10.1007/s00213-022-06099-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-022-06099-4