Abstract
Summary
The epidemiological data on osteogenesis imperfecta (OI) in Asia is limited. This study, representing the first comprehensive epidemiological investigation on OI in Taiwan, reveals high medical resource utilization and underscores the importance of early diagnosis to enhance care quality.
Introduction
This study examines osteogenesis imperfecta, a hereditary connective tissue disorder causing pediatric fractures and limb deformities, using a nationwide database from Taiwan to analyze clinical features and medical burden.
Methods
The study identified validated OI patients from the Catastrophic Illness Registry in the National Health Insurance Research Database from 2008 to 2019. Demographic data and medical resource utilization were analyzed. A multivariate Cox model assessed the influence of sex, validation age, and comorbidities.
Results
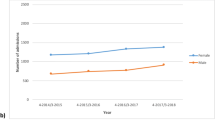
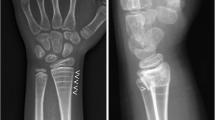
319 OI patients (M/F = 153/166) were identified, with 58% validated before age 20. Prevalence and incidence were 0.8–1.3/100,000 and 0.02–0.09/100,000, respectively, with higher rates in the pediatric demographic. In the study period, 69.6% of the patients had admission history, primarily to pediatric and orthopedic wards. The median admission number was 3, with a median length of stay of 12 days and a median inpatient cost of approximately 3,163 USD during the period. Lower limb fractures were the main reason for hospitalization. 57% of OI patients received bisphosphonate treatment. The leading causes of mortality were OI-related deaths, neurovascular disease, and cardiovascular disease. The median age of validation in the non-survival group was significantly higher compared to the survival group (33 vs. 14 years), and patients validated during childhood required more inpatient fracture surgeries than those validated during adulthood.
Conclusion
This study provides comprehensive real-world evidence on the clinical characteristics and high medical resource utilization of OI patients in a low prevalence region like Taiwan. Early diagnosis is crucial for improving care quality and enhancing health outcomes.



Similar content being viewed by others
Data availability
All data presented in the manuscript can be found in Taiwan’s National Health Insurance Research Database (NHIRD).
References
Van Dijk FS, Sillence DO (2014) Osteogenesis imperfecta: clinical diagnosis, nomenclature and severity assessment. Am J Med Genet Part A 164a:1470–1481
Harrington J, Sochett E, Howard A (2014) Update on the evaluation and treatment of osteogenesis imperfecta. Pediatr Clin North Am 61:1243–1257
Storoni S, Treurniet S, Maugeri A, Pals G, van den Aardweg JG, van der Pas SL, Elting MW, Kloen P, Micha D, Eekhoff EMW (2022) Prevalence and hospital admissions in patients with osteogenesis imperfecta in The Netherlands: a nationwide registry study. Front Endocrinol 13:869604
Gimeno-Martos S, Pérez-Riera C, Guardiola-Vilarroig S, Cavero-Carbonell C (2017) Epidemiology of imperfect osteogenesis: a rare disease in the Valencia Region. Rev Esp Salud Publica 91:e201711045
Binh HD, Maasalu K, Dung VC et al (2017) The clinical features of osteogenesis imperfecta in Vietnam. Int Orthop 41:21–29
Folkestad L (2018) Mortality and morbidity in patients with osteogenesis imperfecta in Denmark. Dan Med J 65:B5454
Sillence DO, Senn A, Danks DM (1979) Genetic heterogeneity in osteogenesis imperfecta. J Med Genet 16:101–116
Forlino A, Marini JC (2016) Osteogenesis imperfecta. Lancet (London, England) 387:1657–1671
Forlino A, Cabral WA, Barnes AM, Marini JC (2011) New perspectives on osteogenesis imperfecta. Nat Rev Endocrinol 7:540–557
Darbà J, Marsà A (2020) Hospital incidence, management and direct cost of osteogenesis imperfecta in Spain: a retrospective database analysis. J Med Econ 23:1435–1440
Kolovos S, Javaid MK, Pinedo-Villanueva R (2021) Hospital admissions of patients with osteogenesis imperfecta in the English NHS. Osteoporos Int 32:1207–1216
Folkestad L, Hald JD, Canudas-Romo V, Gram J, Hermann AP, Langdahl B, Abrahamsen B, Brixen K (2016) Mortality and causes of death in patients with osteogenesis imperfecta: a register-based nationwide cohort study. J Bone Min Res: Off J Am Soc Bone Min Res 31:2159–2166
Folkestad L, Hald JD, Ersbøll AK, Gram J, Hermann AP, Langdahl B, Abrahamsen B, Brixen K (2017) Fracture rates and fracture sites in patients with osteogenesis imperfecta: a nationwide register-based cohort study. J Bone Min Res: Off J Am Soc Bone Min Res 32:125–134
Folkestad L, Hald JD, Gram J, Langdahl BL, Hermann AP, Diederichsen AC, Abrahamsen B, Brixen K (2016) Cardiovascular disease in patients with osteogenesis imperfecta - a nationwide, register-based cohort study. Int J Cardiol 225:250–257
Hsieh CY, Su CC, Shao SC, Sung SF, Lin SJ, Kao Yang YH, Lai EC (2019) Taiwan’s national health insurance research database: past and future. Clin Epidemiol 11:349–358
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Kuitunen I, Ponkilainen VT, Uimonen MM, Eskelinen A, Reito A (2021) Testing the proportional hazards assumption in cox regression and dealing with possible non-proportionality in total joint arthroplasty research: methodological perspectives and review. BMC Musculoskelet Disord 22:489
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 46:399–424
Navani SV, Sarzin B (1967) Intra-uterine osteogenesis imperfecta. Review of the literature and a report of the radiological and necropsy findings in two cases. Br J Radiol 40:449–452
Paterson CR, McAllion S, Stellman JL (1984) Osteogenesis imperfecta after the menopause. N Engl J Med 310:1694–1696
Mai HT, Tran TS, Ho-Le TP, Center JR, Eisman JA, Nguyen TV (2019) Two-thirds of all fractures are not attributable to osteoporosis and advancing age: implications for fracture prevention. J Clin Endocrinol Metab 104:3514–3520
Nijhuis W, Verhoef M, van Bergen C, Weinans H, Sakkers R (2022) Fractures in osteogenesis imperfecta: pathogenesis, treatment, rehabilitation and prevention. Children (Basel, Switzerland) 9:268
Deguchi M, Tsuji S, Katsura D, Kasahara K, Kimura F, Murakami T (2021) Current overview of osteogenesis imperfecta. Medicina (Kaunas, Lithuania) 57:464
Dwan K, Phillipi CA, Steiner RD, Basel D (2016) Bisphosphonate therapy for osteogenesis imperfecta. Cochrane Database Syst Rev 0:Cd005088
Hald JD, Evangelou E, Langdahl BL, Ralston SH (2015) Bisphosphonates for the prevention of fractures in osteogenesis imperfecta: meta-analysis of placebo-controlled trials. J Bone Miner Res 30:929–933
Peddada KV, Sullivan BT, Margalit A, Sponseller PD (2018) Fracture patterns differ between osteogenesis imperfecta and routine pediatric fractures. J Pediatr Orthop 38:e207–e212
Liu W, Lee B, Nagamani SCS, Nicol L, Rauch F, Rush ET, Sutton VR, Orwoll E (2023) Approach to the patient: pharmacological therapies for fracture risk reduction in adults with osteogenesis imperfecta. J Clin Endocrinol Metab 108:1787–1796
Acknowledgements
We are grateful to the Health Data Science Center, National Cheng Kung University Hospital, for providing administrative and technical support.
Funding
The study received support from the National Science and Technology Council (Ministry of Science and Technology) under grant numbers MOST 108–2314-B-006–043-MY2 and MOST 110–2314-B-006–054-MY2 (recipient: CH Wu); NSTC 112–2314-B-006–072 (recipient: CJ Lin); and NSTC 111–2314-B-006–117 (recipient: CA Shih). Additionally, it was supported by the National Cheng Kung University Hospital under grant number NCKUH-11303051 (recipient: CA Shih).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
The study was approved by the Institutional Review Board (IRB) of the National Cheng Kung University Hospital (NCKUH) (IRB No. B-ER-109–416) and ClinicalTrials.gov (No. NCT05367115).
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shih, CA., Li, CC., Chang, YF. et al. Demographics and medical burden of osteogenesis imperfecta: a nationwide database analysis. Osteoporos Int (2024). https://doi.org/10.1007/s00198-024-07051-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00198-024-07051-2