Abstract
Introduction
Osteoporosis has been linked to atherosclerotic diseases such as coronary heart disease and ischemic stroke. However, the relationship between osteoporosis and peripheral artery disease (PAD) has not been investigated. This study aims to evaluate the risk of PAD in patients with osteoporosis and the impact of sex on this association.
Methods
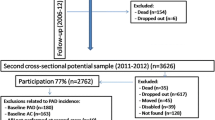
This population-based study used the Longitudinal Health Insurance Database 2005, a subset of Taiwan’s National Health Insurance research database. A total of 54,324 individuals between 40 and 79 years old were included in this study. The osteoporosis group (n = 27,162) consisted of patients with a diagnosis of osteoporosis between January 1, 2002, and December 31, 2006, while the non-osteoporosis group were patients without osteoporosis selected by stratified random sampling (n = 27,162). The primary outcome was the occurrence of newly diagnosed PAD. Cox proportional hazard regression modeling was used to evaluate the association between osteoporosis and the risk of PAD, with adjustment for the baseline characteristics.
Results
The risk of PAD for the osteoporosis group was 28% higher than for the non-osteoporosis group (adjusted hazard ratio (HR) 1.28, 95% confidence interval [CI] 1.20–1.36, p < 0.001), and the PAD-free survival rate was lower in the osteoporosis group (p < 0.001). Sex-stratified analysis revealed a similar HR magnitude between osteoporotic men (HR 1.36; 95% CI 1.19–1.57) and women (HR 1.25; 95% CI 1.17–1.35), compared with their non-osteoporotic counterparts.
Conclusion
This study found an increased long-term risk of PAD in both men and women with osteoporosis.
Mini abstract
Osteoporosis has been associated with increased risks of atherosclerotic diseases. However, the relationship between osteoporosis and peripheral artery disease remains uncertain. The present population-based longitudinal follow-up study showed that patients with osteoporosis are at an increased risk of developing peripheral artery disease.


Similar content being viewed by others
Data availability
The data generated and analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1767. https://doi.org/10.1016/s0140-6736(02)08657-9
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136. https://doi.org/10.1007/s11657-013-0136-1
Szekanecz Z, Raterman HG, Pethő Z, Lems WF (2019) Common mechanisms and holistic care in atherosclerosis and osteoporosis. Arthritis Res Ther 21:15. https://doi.org/10.1186/s13075-018-1805-7
Duff S, Mafilios MS, Bhounsule P, Hasegawa JT (2019) The burden of critical limb ischemia: a review of recent literature. Vasc Health Risk Manag 15:187–208. https://doi.org/10.2147/vhrm.S209241
Hu X, Ma S, Yang C, Wang W, Chen L (2019) Relationship between senile osteoporosis and cardiovascular and cerebrovascular diseases. Exp Ther Med 17:4417–4420. https://doi.org/10.3892/etm.2019.7518
Nordström A, Eriksson M, Stegmayr B, Gustafson Y, Nordström P (2010) Low bone mineral density is an independent risk factor for stroke and death. Cerebrovasc Dis 29:130–136. https://doi.org/10.1159/000262308
Baldwin MJ, Policha A, Maldonado T, Hiramoto JS, Honig S, Conte MS, Berger J, Rockman CB (2017) Novel association between bone mineral density scores and the prevalence of peripheral artery disease in both sexes. Vasc Med 22:13–20. https://doi.org/10.1177/1358863x16672740
van der Klift M, Pols HA, Hak AE, Witteman JC, Hofman A, de Laet CE (2002) Bone mineral density and the risk of peripheral arterial disease: the Rotterdam Study. Calcif Tissue Int 70:443–449. https://doi.org/10.1007/s00223-001-2076-9
Farhat GN, Strotmeyer ES, Newman AB, Sutton-Tyrrell K, Bauer DC, Harris T, Johnson KC, Taaffe DR, Cauley JA (2006) Volumetric and areal bone mineral density measures are associated with cardiovascular disease in older men and women: the health, aging, and body composition study. Calcif Tissue Int 79:102–111. https://doi.org/10.1007/s00223-006-0052-0
Lee YC, Huang YT, Tsai YW, Huang SM, Kuo KN, McKee M, Nolte E (2010) The impact of universal National Health Insurance on population health: the experience of Taiwan. BMC Health Serv Res 10:225. https://doi.org/10.1186/1472-6963-10-225
Pande RL, Creager MA (2014) Socioeconomic inequality and peripheral artery disease prevalence in US adults. Circ Cardiovasc Qual Outcomes 7:532–539. https://doi.org/10.1161/circoutcomes.113.000618
Liu CY, Hung YT, Chuang YL, Chen YJ, Weng WS, Liu JS, Liang K (2006) Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J Health Manag 4:1–22
Wu CY, Chen YJ, Ho HJ, Hsu YC, Kuo KN, Wu MS, Lin JT (2012) Association between nucleoside analogues and risk of hepatitis B virus–related hepatocellular carcinoma recurrence following liver resection. JAMA 308:1906–1914. https://doi.org/10.1001/2012.jama.11975
de Pablo P, Cooper MS, Buckley CD (2012) Association between bone mineral density and C-reactive protein in a large population-based sample. Arthritis Rheum 64:2624–2631. https://doi.org/10.1002/art.34474
Scheidt-Nave C, Bismar H, Leidig-Bruckner G, Woitge H, Seibel MJ, Ziegler R, Pfeilschifter J (2001) Serum interleukin 6 is a major predictor of bone loss in women specific to the first decade past menopause. J Clin Endocrinol Metab 86:2032–2042. https://doi.org/10.1210/jcem.86.5.7445
Zha L, He L, Liang Y, Qin H, Yu B, Chang L, Xue L (2018) TNF-α contributes to postmenopausal osteoporosis by synergistically promoting RANKL-induced osteoclast formation. Biomedicine & Pharmacotherapy 102:369–374. https://doi.org/10.1016/j.biopha.2018.03.080
Redlich K, Smolen JS (2012) Inflammatory bone loss: pathogenesis and therapeutic intervention. Nat Rev Drug Discov 11:234–250. https://doi.org/10.1038/nrd3669
Tzoulaki I, Murray GD, Lee AJ, Rumley A, Lowe GD, Fowkes FG (2005) C-reactive protein, interleukin-6, and soluble adhesion molecules as predictors of progressive peripheral atherosclerosis in the general population: Edinburgh Artery Study. Circulation 112:976–983. https://doi.org/10.1161/circulationaha.104.513085
Pande RL, Brown J, Buck S, Redline W, Doyle J, Plutzky J, Creager MA (2015) Association of monocyte tumor necrosis factor α expression and serum inflammatory biomarkers with walking impairment in peripheral artery disease. J Vasc Surg 61:155–161. https://doi.org/10.1016/j.jvs.2014.06.116
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281. https://doi.org/10.1056/NEJMra070553
Narula R, Tauseef M, Ahmad IA, Agarwal K, Ashok A, Anjana A (2013) Vitamin d deficiency among postmenopausal women with osteoporosis. J Clin Diagn Res 7:336–338. https://doi.org/10.7860/jcdr/2013/5022.2761
Haas MJ, Jafri M, Wehmeier KR, Onstead-Haas LM, Mooradian AD (2016) Inhibition of endoplasmic reticulum stress and oxidative stress by vitamin D in endothelial cells. Free Radic Biol Med 99:1–10. https://doi.org/10.1016/j.freeradbiomed.2016.07.020
Oh J, Weng S, Felton SK et al (2009) 1,25(OH)2 vitamin d inhibits foam cell formation and suppresses macrophage cholesterol uptake in patients with type 2 diabetes mellitus. Circulation 120:687–698. https://doi.org/10.1161/circulationaha.109.856070
Melamed ML, Muntner P, Michos ED, Uribarri J, Weber C, Sharma J, Raggi P (2008) Serum 25-hydroxyvitamin D levels and the prevalence of peripheral arterial disease: results from NHANES 2001 to 2004. Arterioscler Thromb Vasc Biol 28:1179–1185. https://doi.org/10.1161/atvbaha.108.165886
Lu Y, Ballew SH, Kwak L, Selvin E, Kalbaugh CA, Schrack JA, Matsushita K, Szklo M (2019) Physical activity and subsequent risk of hospitalization with peripheral artery disease and critical limb ischemia in the ARIC study. J Am Heart Assoc 8:e013534. https://doi.org/10.1161/jaha.119.013534
Sallam N, Laher I (2016) Exercise modulates oxidative stress and inflammation in aging and cardiovascular diseases. Oxid Med Cell Longev 2016:7239639. https://doi.org/10.1155/2016/7239639
Pagnotti GM, Styner M, Uzer G, Patel VS, Wright LE, Ness KK, Guise TA, Rubin J, Rubin CT (2019) Combating osteoporosis and obesity with exercise: leveraging cell mechanosensitivity. Nat Rev Endocrinol 15:339–355. https://doi.org/10.1038/s41574-019-0170-1
Meyer F, König HH, Hajek A (2019) Osteoporosis, fear of falling, and restrictions in daily living. Evidence from a nationally representative sample of community-dwelling older adults. Front Endocrinol (Lausanne) 10:646. https://doi.org/10.3389/fendo.2019.00646
Tonelli M, Wiebe N, Fortin M et al (2015) Methods for identifying 30 chronic conditions: application to administrative data. BMC Med Inform Decis Mak 15:31. https://doi.org/10.1186/s12911-015-0155-5
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Not applicable
Consent to participate
Not applicable
Consent for publication
Consent for submission and publication has been received from all authors.
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liang, YS., Yeh, KC. & Pan, SL. Osteoporosis and the long-term risk of peripheral artery disease: a population-based longitudinal follow-up study in Taiwan. Osteoporos Int 33, 1117–1123 (2022). https://doi.org/10.1007/s00198-022-06305-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06305-1