Abstract
Introduction and hypothesis
The aim of this review is to discuss the link between menopause and nocturia and to give an overview of the increasing prevalence, risk factors, causative factors, treatment needs and options for nocturia in peri-menopausal women.
Methods
This opinion article is a narrative review based on the expertise and consensus of a variety of key opinion leaders, in combination with an extensive literature review. This literature search included a thorough analysis of potential publications on both the PubMed Database and the Web of Science and was conducted between November 2022 and December 2022. The following key words were used “nocturia” and “menopause” or “nocturnal frequency and menopause.” Moreover, key words including “incidence,” “prevalence,” “insomnia,” “estrogen therapy,” “metabolic syndrome,” and “hot flushes” were used in combination with the aforementioned key words. Last, the reference lists of articles obtained were screened for other relevant literature.
Results
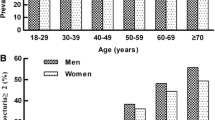
The perimenopause can be a trigger for inducing nocturia. Typically, obesity, body mass index (BMI), and waist circumference are risk factors for developing peri-menopausal nocturia. Presumably the development of peri-menopausal nocturia is multifactorial, with interplay among bladder, sleep, and kidney problems due to estrogen depletion after the menopause. First, impaired stimulation of estrogen receptors in the urogenital region leads to vaginal atrophy and reduced bladder capacity. Moreover, menopause is associated with an increased incidence of overactive bladder syndrome. Second, estrogen deficiency can induce salt and water diuresis through blunted circadian rhythms for the secretion of antidiuretic hormone and the activation of the renin–angiotensin–aldosterone system. Additionally, an increased incidence of sleep disorders, including vasomotor symptoms and obstructive sleep apnea signs, is observed. Oral dryness and a consequent higher fluid intake are common peri-menopausal symptoms. Higher insulin resistance and a higher risk of cardiovascular diseases may provoke nocturia. Given the impact of nocturia on general health and quality of life, bothersome nocturia should be treated. Initially, behavioral therapy should be advised. If these modifications are inadequate, specific treatment should be proposed. Systemic hormone replacement is found to have a beneficial effect on nocturia, without influencing sodium and water clearance in patients with nocturnal polyuria. It is presumed that the improvement in nocturia from hormonal treatment is due to an improvement in sleep disorders.

Similar content being viewed by others
Abbreviations
- ADH:
-
Antidiuretic hormone
- AT:
-
Adipose tissue
- ANP:
-
Atrial natriuretic peptide
- BMI:
-
Body mass index
- BNP:
-
Brain natriuretic peptides
- BOO:
-
Bladder outlet obstruction
- CKI:
-
Chronic kidney injury
- CVD:
-
Cardiovascular disease
- GFR:
-
Glomerular filtration rate
- GSM:
-
Genitourinary symptoms of the menopause
- HFs:
-
Hot flashes
- HRT:
-
Hormonal replacement treatment
- ICS:
-
International Continence Society
- LUTS:
-
Lower urinary tract symptom
- MetS:
-
Metabolic syndrome
- NP:
-
Nocturnal polyuria
- OAB:
-
Overactive bladder
- OSAS:
-
Obstructive sleep apnea syndrome
- RAAS:
-
Renin–angiotensin–aldosterone system
- UTI:
-
Urinary tract infection
- VMS:
-
Vasomotor symptoms
References
Hashim H, Blanker MH, Drake MJ, et al. International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol Urodyn. 2019; 38:499–508.
Andersson F, Anderson P, Holm-Larsen T, Piercy J, Everaert K, Holbrook T. Assessing the impact of nocturia on health-related quality-of-life and utility: results of an observational survey in adults. J Med Econ. 2016;19:1200–6. https://doi.org/10.1080/13696998.2016.1211136.
Tikkinen KAO, Johnson TM, Tammela TLJ, et al. Nocturia frequency, bother, and quality of life: how often is too often? A population-based study in Finland. Eur Urol. 2010;57:488–98..
Vaughan CP, Fung CH, Huang AJ, Johnson TM, Markland AD. Differences in the association of nocturia and functional outcomes of sleep by age and gender: a cross-sectional, population-based study. Clin Ther. 2016;38:2386–93.e1.
Pauwaert K, Bruneel E, van Laecke E, Depypere H, Everaert K, Goessaert AS. Does hormonal therapy affect the bladder or the kidney in postmenopausal women with and without nocturnal polyuria: results of a pilot trial? Maturitas. 2022;160:61–7.
Everaert K, Hervé F, Bosch R, et al. International Continence Society consensus on the diagnosis and treatment of nocturia. Neurourol Urodyn. 2019;38:478–98. https://doi.org/10.1002/nau.23939.
Varella LRD, Bezerra da Silva R, Eugênia de Oliveira MC, et al. Assessment of lower urinary tract symptoms in different stages of menopause. J Phys Ther Sci. 2016;28:3116–21.
Harlow SD, Gass M, Hall JE, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. Menopause. 2012;19:1.
Hsu A, Nakagawa S, Walter LC, et al. The burden of nocturia among middle-aged and older women. Obstet Gynecol. 2015;125:35–43.
Rekers H, Drogendijk AC, Valkenburg HA, Riphagen F. The menopause, urinary incontinence and other symptoms of the genito-urinary tract. Maturitas. 1992;15:101–11.
Srisukho S, Pantasri T, Piyamongkol W, Phongnarisorn C, Morakote N. The experience of genitourinary syndrome of menopause (GSM) among Thai postmenopausal women: the non-reporting issue. Int Urogynecol J. 2019;30:1843–7.
Jones HJ, Huang AJ, Subak LL, Brown JS, Lee KA. Bladder symptoms in the early menopausal transition. J Womens Health (Larchmt). 2016;25:457–63.
Tikkinen KAO, Auvinen A, Tiitinen A, Valpas A, Johnson TM, Tammela TLJ. Reproductive factors associated with nocturia and urinary urgency in women: a population-based study in Finland. Am J Obstet Gynecol. 2008;199:153.e1–12.
Tikkinen KAO, Johnson TM, Tammela TLJ, et al. Nocturia frequency, bother, and quality of life: how often is too often? A population-based study in Finland. Eur Urol. 2010;57:488–96.
Asplund R, Åberg HE. Nocturia and health in women aged 40–64 years. Maturitas. 2000;35:143–8.
Chen YC, den Chen G, Hu SW, Lin TL, Lin LY. Is the occurrence of storage and voiding dysfunction affected by menopausal transition or associated with the normal aging process? Menopause. 2003;10:203–8.
Pauwaert K, Goessaert A-S, Ghijselings L, Bower W, Depypere H, Everaert K. Characterizing nocturia among Belgian healthy postmenopausal women: prevalence, bother, etiology and possible risk factors for developing nocturia. Maturitas. 2020;143:41–6.
Terauchi M, Hirose A, Akiyoshi M, Owa Y, Kato K, Kubota T. Prevalence and predictors of storage lower urinary tract symptoms in perimenopausal and postmenopausal women attending a menopause clinic. Menopause. 2015;22:1084–90.
Nakagawa H, Niu K, Hozawa A, et al. Impact of nocturia on bone fracture and mortality in older individuals: a Japanese longitudinal cohort study. J Urol. 2010;184:1413–8.
Tang R, Fan Y, Luo M, et al. General and central obesity are associated with increased severity of the VMS and sexual symptoms of menopause among Chinese women: a longitudinal study. Front Endocrinol (Lausanne). 2022;13:814872.
Hetemäki N, Savolainen-Peltonen H, Tikkanen MJ, et al. Estrogen metabolism in abdominal subcutaneous and visceral adipose tissue in postmenopausal women. J Clin Endocrinol Metab. 2017;102:4588–95.
Lizcano F. Roles of estrogens, estrogen-like compounds, and endocrine disruptors in adipocytes. Front Endocrinol (Lausanne). 2022;13:921504.
Pauwaert K, Goessaert A-S, Ghijselings L, et al. Hormone therapy as a possible solution for postmenopausal women with nocturia. Menopause. 2021;28:502–10.
Everaert K, Hervé F, Bower W, Djurhuus JC, Dmochowski R, Fine N, et al. How can we develop a more clinically useful and robust algorithm for diagnosing and treating nocturia? ICI-RS 2017. Neurourol Urodyn. 2018;37:S46–59.
Bower WF, Rose GE, Whishaw DM, Ervin CF, Wang AC, Moore KH. The association between nocturia, hormonal symptoms and bladder parameters in women: an observational study. BJOG. 2022;129:812–9.
Leimola-Virtanen R, Salo T, Toikkanen S, Pulkkinen J, Syrjänen S. Expression of estrogen receptor (ER) in oral mucosa and salivary glands. Maturitas. 2000;36:131–7.
Minicucci EM, Pires RBC, Vieira RA, Miot HA, Sposto MR. Assessing the impact of menopause on salivary flow and xerostomia. Aust Dent J. 2013;58:230–4.
Asplund R, Åberg HE. Oral dryness, nocturia and the menopause. Maturitas. 2005;50:86–90.
Chagnac A. The effects of weight loss on renal function in patients with severe obesity. J Am Soc Nephrol. 2003;14:1480–6. https://doi.org/10.1097/01.ASN.0000068462.38661.89.
Cardozo L, Robinson D, Dmochowski RR, et al. Special considerations in premenopausal and postmenopausal women with symptoms of overactive bladder. Urology. 2002;60:64–71; discussion 71.
Blümel JE, Chedraui P, Baron G, et al. Menopausal symptoms appear before the menopause and persist 5 years beyond: a detailed analysis of a multinational study. Climacteric. 2012;15:542–51.
Portman DJ, Gass MLS, Kingsberg S, et al. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21:1063–8.
Robinson D, Toozs-Hobson P, Cardozo L. The effect of hormones on the lower urinary tract. Menopause Int. 2013;19:155–62.
Pfisterer MH-D, Griffiths DJ, Rosenberg L, Schaefer W, Resnick NM. Parameters of bladder function in pre-, peri-, and postmenopausal continent women without detrusor overactivity. Neurourol Urodyn. 2007;26:356–61.
Parsons M, Amundsen CL, Cardozo L, Vella M, Webster GD, Coats AC. Bladder diary patterns in detrusor overactivity and urodynamic stress incontinence. Neurourol Urodyn. 2007;26:800–6. https://doi.org/10.1002/nau.20406.
Hristov KL, Parajuli SP, Provence A, Rovner ES, Petkov GV. Nongenomic modulation of the large conductance voltage- and Ca2+-activated K+ channels by estrogen: a novel regulatory mechanism in human detrusor smooth muscle. Physiol Rep. 2017;5:e13351.
Potier M, Karl M, Zheng F, Elliot SJ, Striker GE, Striker LJ. Estrogen-related abnormalities in glomerulosclerosis-prone mice: reduced mesangial cell estrogen receptor expression and prosclerotic response to estrogens. Am J Pathol. 2002;160:1877–85.
Potier M, Elliot SJ, Tack I, et al. Expression and regulation of estrogen receptors in mesangial cells: influence on matrix metalloproteinase-9. J Am Soc Nephrol. 2001;12:241–51.
Oelkers WHK. Drospirenone in combination with estrogens: for contraception and hormone replacement therapy. Climacteric. 2005;8:19–27. https://doi.org/10.1080/13697130500330341.
Forsling ML, Akerlund M, Stromberg P. Variations in plasma concentrations of vasopressin during the menstrual cycle. J Endocrinol. 1981;89:263–6.
Goessaert A-S, vande Walle J, Kapila A, Everaert K. Hormones and nocturia: guidelines for medical treatment? J Steroids Horm Sci. 2014. https://doi.org/10.4172/2157-7536.1000130.
Tani M, Hirayama A, Fujimoto K, Torimoto K, Akiyama T, Hirao Y. Increase in 24-hour urine production/weight causes nocturnal polyuria due to impaired function of antidiuretic hormone in elderly men. Int J Urol. 2008;15:151–4.
Graugaard-Jensen C, Hvistendahl GM, Frøkiær J, Bie P, Djurhuus JC. The influence of high and low levels of estrogen on diurnal urine regulation in young women. BMC Urol. 2008;8:16.
Stachenfeld NS, DiPietro L, Palter SF, Nadel ER. Estrogen influences osmotic secretion of AVP and body water balance in postmenopausal women. Am J Physiol Regul Integr Comp Physiol. 1998;274:R187–95.
Oelkers WKH. Effects of estrogens and progestogens on the renin-aldosterone system and blood pressure. Steroids. 1996;61:166–71.
Kolatorova L, Vitku J, Suchopar J, Hill M, Parizek A. Progesterone: a steroid with wide range of effects in physiology as well as human medicine. Int J Mol Sci. 2022;23:7989.
Komukai K, Mochizuki S, Yoshimura M. Gender and the renin-angiotensin-aldosterone system. Fundam Clin Pharmacol. 2010;24:687–98.
Bossmar T, Forsling M, Åkerlund M. Circulating oxytocin and vasopressin is influenced by ovarian steroid replacement in women. Acta Obstet Gynecol Scand. 1995;74:544–8.
Jeong HG, Park H. Metabolic disorders in menopause. Metabolites. 2022;12:954.
Tom SE, Kuh D, Guralnik JM, Mishra GD. Self-reported sleep difficulty during the menopausal transition: results from a prospective cohort study. Menopause. 2010;17:1128–35.
Kravitz HM, Zhao X, Bromberger JT, et al. Sleep disturbance during the menopausal transition in a multi-ethnic community sample of women. Sleep. 2008;31:979.
Dennerstein L, Lehert P, Guthrie JR, Burger HG. Modeling women’s health during the menopausal transition: a longitudinal analysis. Menopause. 2007;14:53–62.
Freedman RR. Hot flashes: behavioral treatments, mechanisms, and relation to sleep. Am J Med. 2005;118:124–30.
Kravitz HM, Ganz PA, Bromberger J, Powell LH, Sutton-Tyrrell K, Meyer PM. Sleep difficulty in women at midlife: a community survey of sleep and the menopausal transition. Menopause. 2003;10:19–28.
Kapsimalis F, Kryger M. Sleep breathing disorders in the U.S. female population. J Womens Health (Larchmt). 2009;18:1211–9.
Bixler EO, Vgontzas AN, Lin HM, et al. Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med. 2001;163:608–13. https://doi.org/10.1164/ajrccm.163.3.9911064.
Shepertycky MR, Banno K, Kryger MH. Differences between men and women in the clinical presentation of patients diagnosed with obstructive sleep apnea syndrome. Sleep. 2005;28:309–14.
Dancey DR, Hanly PJ, Soong C, Lee B, Hoffstein V. Impact of menopause on the prevalence and severity of sleep apnea. Chest. 2001;120:151–5.
Young T, Finn L, Austin D, Peterson A. Menopausal status and sleep-disordered breathing in the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med. 2003;167:1181–5. https://doi.org/10.1164/rccm.200209-1055OC.
Umlauf MG, Chasens ER, Greevy RA, Arnold J, Burgio KL, Pillion DJ. Obstructive sleep apnea, nocturia and polyuria in older adults. Sleep. 2004;27:139–44.
Hirayama A, Torimoto K, Yamada A, Tanaka N, Fujimoto K, Yoshida K, et al. Relationship between nocturnal urine volume, leg edema, and urinary antidiuretic hormone in older men. Urology. 2011;77:1426–31.
Torimoto K, Hirayama A, Samma S, Yoshida K, Fujimoto K, Hirao Y. The relationship between nocturnal polyuria and the distribution of body fluid: assessment by bioelectric impedance analysis. J Urol. 2009;181:219–24.
Wali MA, Raparelli V, Pilote L, Daskalopoulou SS. Blood pressure variability in normotensive perimenopausal women: non-dipping status, maximum blood pressure and arterial stiffness. Int J Cardiol. 2021;325:149–54.
McKeigue PM, Reynard JM. Relation of nocturnal polyuria of the elderly to essential hypertension. Lancet. 2000;355:486–8. https://doi.org/10.1016/S0140-6736(00)82039-5.
Carpenter J, Gass MLS, Maki PM, et al. Nonhormonal management of menopause-associated vasomotor symptoms. Menopause. 2015;22:1155–74.
Harding CK, Lapitan MC, Bø K, et al. EAU Guidelines on the management of non-neurogenic female lower urinary tract symptoms (LUTS). EAU Guidelines. Presented at the EAU Annual Congress Milan 2021; 2020.
Weiss JP. Nocturia: focus on etiology and consequences. Rev Urol. 2012;14:48–55.
Hanna-Mitchell AT, Robinson D, Cardozo L, Everaert K, Petkov GV. Do we need to know more about the effects of hormones on lower urinary tract dysfunction? ICI-RS 2014. Neurourol Urodyn. 2016;35:299–303.
Weiss JP, Everaert K. Management of nocturia and nocturnal polyuria. Urology. 2019;133:24–33. https://doi.org/10.1016/j.urology.2019.09.022.
Oelke M, de Wachter S, Drake MJ, Giannantoni A, Kirby M, Orme S, et al. A practical approach to the management of nocturia. Int J Clin Pract. 2017;71(11):e13027. https://doi.org/10.1111/ijcp.13027.
Miyauchi Y, Okazoe H, Okujyo M, et al. Effect of the continuous positive airway pressure on the nocturnal urine volume or night-time frequency in patients with obstructive sleep apnea syndrome. Urology. 2015;85:333–6.
Ghijselings L, Hervé F, Van der Aa F, et al. Development of a flowchart reflecting the current attitude and approach towards idiopathic overactive bladder treatment in Belgium: a Delphi study. Neurourol Urodyn. 2020;39:1781–95https://doi.org/10.1002/nau.24421.
Margel D, Shochat T, Getzler O, Livne PM, Pillar G. Continuous positive airway pressure reduces nocturia in patients with obstructive sleep apnea. Urology. 2006;67:974–7.
Viaene A, Roggeman S, Goessaert AS, et al. Conservative treatment for leg oedema and the effect on nocturnal polyuria in patients with spinal cord injury. BJU Int. 2019;123:E43–50.
Juul KV, Bichet DG, Nielsen S, Nørgaard JP. The physiological and pathophysiological functions of renal and extrarenal vasopressin V2 receptors. Am J Physiol Renal Physiol. 2014;306:F931–40.
Long CY, Liu CM, Hsu SC, Chen YH, Wu CH, Tsai EM. A randomized comparative study of the effects of oral and topical estrogen therapy on the lower urinary tract of hysterectomized postmenopausal women. Fertil Steril. 2006;85:155–60.
Santen RJ. Vaginal administration of estradiol: effects of dose, preparation and timing on plasma estradiol levels. Climacteric. 2015;18:121–34. https://doi.org/10.3109/13697137.2014.947254.
The 2017 hormone therapy position statement of the North American Menopause Society. Menopause. 2018;25:1362–87.
Cardozo L, Lose G, McClish D, Versi E. A systematic review of the effects of estrogens for symptoms suggestive of overactive bladder. Acta Obstet Gynecol Scand. 2004;83:892–7.
Reynard JM, Cannon A, Yang Q, Abrams P. A novel therapy for nocturnal polyuria: a double-blind randomized trial of frusemide against placebo. Br J Urol. 1998;81:215–8. https://doi.org/10.1046/j.1464-410X.1998.00511.x.
Miyazato M, Tohyama K, Touyama M, et al. Effect of continuous positive airway pressure on nocturnal urine production in patients with obstructive sleep apnea syndrome. Neurourol Urodyn. 2017;36:376–9. https://doi.org/10.1002/nau.22936.
Rahn DD, Carberry C, Sanses TV, et al. Vaginal estrogen for genitourinary syndrome of menopause. Obstet Gynecol. 2014;124:1147–56.
Cistulli PA, Barnes DJ, Grunstein RR, et al. Effect of short term hormone replacement in the treatment of obstructive sleep apnoea in postmenopausal women. Thorax. 1994;49:699–702.
Bower WF, Rose GE, Ervin CF, Goldin J, Whishaw DM, Khan F. TANGO—a screening tool to identify comorbidities on the causal pathway of nocturia. BJU Int. 2017;119:933–41.
Rose GE, Bower WF. Development of a scoring process for the nocturia causality screening tool TANGO: a rationale and methodology. Aust N Z Continence J. 2020;26:3.
Decalf V, Everaert K, de Witte N, Petrovic M, Bower W. Dutch version of the TANGO nocturia screening tool: cross-culturally translation and reliability study in community-dwelling people and nursing home residents. Acta Clin Belg. 2020;75(6):397–404.
Pauwaert K, Goessaert AS, Ghijselings L, Monaghan TF, Depypere H, Everaert K. Nocturia through the menopausal transition and beyond: a narrative review. Int Urogynecol J. 2021;32:1097–106.
Kok ALM, Burger CW, van de Weijer PHM, Voetberg GA, Peters-Muller ERA, Kenemans P. Micturition complaints in postmenopausal women treated with continuously combined hormone replacement therapy: a prospective study. Maturitas. 1999;31:143–9.
Leimola-Virtanen R, Helenius H, Laine M. Hormone replacement therapy and some salivary antimicrobial factors in post- and perimenopausal women. Maturitas. 1997;27:145–51.
MacLennan AH, Broadbent JL, Lester S, Moore V. Oral oestrogen and combined oestrogen/progestogen therapy versus placebo for hot flushes. Cochrane Database Syst Rev. 2004;2004:CD002978.
Shahar E, Redline S, Young T, Boland LL, Baldwin CM, Nieto FJ, et al. Hormone replacement therapy and sleep-disordered breathing. Am J Respir Crit Care Med. 2003;167:1186–92.
Author information
Authors and Affiliations
Contributions
Kim Pauwaert: literature search, drafting of the manuscript; An-Sofie Goessaert: general discussion, reviewing of the manuscript; Dudley Robinson: general discussion, reviewing of the manuscript; Linda Cardozo: general discussion, reviewing of the manuscript; Wendy Bower: general discussion, reviewing of the manuscript; Patrick Calders: general discussion, reviewing of the manuscript; An Mariman: general discussion, reviewing of the manuscript; Paul Abrams: general discussion, reviewing of the manuscript; Andrea Tubaro: general discussion, reviewing of the manuscript; Roger Dmochowski: general discussion, reviewing of the manuscript; Jeffrey P. Weiss: general discussion, reviewing of the manuscript; Francois Hervé: general discussion, reviewing of the manuscript; Herman Depypere: general discussion, reviewing of the manuscript; Karel Everaert: general discussion, reviewing of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Dudley Robinson is a speaker for Allergan. Paul Abrams reports being a consultant for Astellas, Teva, and Sandoz. In addition, he is a Speaker for Astellas, Cipla, Ferring, and Sun Pharma. Francois Hervé reports grants from Astellas, Ferring, Apogepha, Coloplast, and Medtronic, outside the submitted work. Karel Everaert reports grants to the institution from Ferring, Astellas, and Medtronic. All the other authors report no conflicts of interest.
Additional information
Handling Editor: Gin-Den Chen
Editor in Chief: Kaven Baessler
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pauwaert, K., Goessaert, AS., Robinson, D. et al. Nocturia in Menopausal Women: The Link Between Two Common Problems of the Middle Age. Int Urogynecol J 35, 935–946 (2024). https://doi.org/10.1007/s00192-024-05743-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-024-05743-1