Abstract
Introduction and hypothesis
This study aimed to compare the effectiveness of a hybrid telerehabilitation program with a traditional face to face model in women with stress urinary incontinence (SUI) and mixed incontinence (MUI) with a predominance of SUI. The authors hypothesized that home pelvic floor muscle training (PFMT) would have a similar benefit to outpatient PFMT.
Methods
Parallel randomized controlled trial including 58 patients consecutively admitted to a tertiary academic hospital for pelvic floor rehabilitation consultation from 1 January to 30 April 2021 for conservative treatment of UI. Participants randomized to the intervention were submitted to a 12-week PFMT program: (1) a hybrid telerehabilitation program of two individual face-to-face sessions followed by 2-weekly sessions of video-telerehabilitation with a follow-up by a specialized physiotherapist, including one individual face-to-face session at 8 weeks; (2) a re-evaluation teleconsultation at 6 and 16 weeks; (3) a face-to-face consultation at 12 weeks. The control group had two initial individual sessions followed by twice-weekly group classes, and consultations were face to face. The primary outcome measure (at baseline and 12 weeks) was UI-related quality of life using the Portuguese Version of the King's Health Questionnaire.
Results
At baseline the intervention (n = 18) and control (n = 17) groups were similar. UI-related quality of life significantly improved in both the intervention and control groups betweenbaseline (T0) and the end of the 12-week PFMT program (T12) (p = 0.002, p < 0.001, respectively), although the magnitude of the improvement was not significantly different between groups (–10.0 vs. –9.5 points, p = 0.918, respectively).
Conclusion
This hybrid telerehabilitation protocol showed effectiveness comparable to the traditional model in improving UI-related quality of life. Trial registration at www.ClinicalTrials.gov, no. NCT05114395.
Similar content being viewed by others
Introduction
Urinary incontinence (UI) is defined, according to the International Continence Society (ICS), as any involuntary loss of urine [1].
It affects 21.4% of Portuguese women, and its prevalence increases with age, having a negative impact on the quality of life and sexual function [2].
The literature concerning the types of UI in women is in agreement and refers to stress urinary incontinence (SUI) as the most prevalent, followed by mixed incontinence (MUI) and urge incontinence (UUI) [3, 4].
Pelvic floor muscle training (PFMT) is the most commonly recommended treatment for women with SUI, in which urine loss occurs with increases in intra-abdominal pressure due to the weakening of the musculotendinous structures of the pelvic floor [5, 6]. It is also used in the treatment of women with MUI and less frequently for UUI [6].
Due to the pandemic caused by coronavirus disease 2019 (COVID-19), telehealth recommendations were released, enhancing the motivation for telerehabilitation, initially represented by the possibility to increase access to health care for the population for which it was otherwise not available (e.g., in rural locations) [7].
Moreover, the authors believe that more ambitious opportunities were present as telerehabilitation may enable not only more convenient delivery of health care even for UI patients who have regular access to the standard health system but also hopefully cost reduction. In addition, in the current context, it can help comply with quarantine strategies to reduce virus diffusion and protect patients and physicians. Recent literature has shown that home PFMT has a similar benefit to outpatient PFMT [7]. Hui et al. showed that videoconferencing is as effective as conventional methods in the management of UI [8].
In a systematic review of the 2020 literature, PFMT combined with behavioral measures via telehealth programs is recommended according to the lastest randomized clinical trials (RCT) published, but no framework has been reported for the implementation of telerehabilitation in PFMT [9]. Furthermore, to our knowledge no study has been published concerning this topic in Portugal.
Therefore, we aimed to compare the effectiveness of a hybrid telerehabilitation program with a conventional face-to-face model in female patients with SUI and MUI with a predominance of SUI, hypothesizing that it would be similar.
Methods
This parallel RCT was conducted among women who fulfilled the following criteria: aged between 18 and 65 years with SUI or MUI with a predominance of SUI with at least one UI episode per week in the last month (their UI was only defined by their predominant symptoms), with pelvic floor muscle strength ≥ 2 on the modified Oxford grading scale (MOS) [10], who were capable of understanding and executing the therapeutic program and expressed willingness to participate in the study with a free and informed written consent.
The allocation sequence was generated by a research assistant using computer-generated random numbers with a 1:1 allocation ratio. The sequence was implemented using sequentially numbered sealed, opaque envelopes. The envelopes were stored in a closed locker in the center to which only the research assistant had access. The envelopes were given to the doctors immediately before the initial individual outpatient session. Participants and health professionals, namely a Physical Medicine and Rehabilitation (PMR) doctor and a physical therapist, both specialized and with > 10 years of pelvic floor rehabilitation experience, were not blinded to the study groups.
Our exclusion criteria included patients with UUI or MUI with a predominance of urgency; active pelvic neoplasia; pelvic organ prolapse grade ≥ 2; active urinary tract infection or macroscopic hematuria; neurogenic dysfunction of the lower urinary tract; cognitive deficit; osteoarticular, neurological or psychiatric pathologies that could prevent the realization of the therapeutic program; conservative or surgical treatment of UI in the last 12 months; pregnant women; the impossibility of access or the illiteracy related to technological means (phone or computer); the unavailability to attend the face-to-face program due to accessibility, schedule, economic reasons or fear of the pandemic context.
Fifty-eight eligible women were invited to participate in this study at their first face-to-face pelvic floor rehabilitation consultation at a tertiary academic hospital between 1 January and 30 April 2021. Twenty-three patients were excluded because of negative ICS (International Continence Society) pad testing (≤ 1 g) [11, 12], comorbidities, pregnancy, muscular strength grade 1 in the MOS, refusal to participate and inability to be contacted.
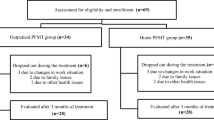
Patient enrollment, allocation, follow-up and implementation of the intervention are shown in Figs. 1 and 2.
Implementation of the intervention. PFMT = pelvic floor muscle training. KHQ = King’s Health Questionnaire. ICIQ-SF = International Consultation on Incontinence Questionnaire-Short Form. FSFI = Female Sexual Function Index. HADS - Hospital Anxiety and Depression Scale. PGI-I = Patient Global Impression of Improvement
The intervention group included a 12-week hybrid telerehabilitation program including two initial individual face-to-face sessions with a specialized therapist followed by 2-weekly video-telerehabilitation sessions and one individual face-to-face session at 8 weeks, also followed by the 2-weekly video-telerehabilitation sessions. In the first medical consultation, a presential one, patients were instructed in behavioral and lifestyle measures and were prescribed the PFMT program. This program consisted not only of the three individual face-to-face sessions mentioned before and the 2-weekly, 30-min telerehabilitation sessions, divided into three phases with the gradual addition of exercises of increasing difficulty in terms of duration, number of repetitions and positions, but also of exercises to be performed three times a day (standing, sitting and lying down) [13]. In the middle of the treatment (at 6 weeks or T6), a medical teleconsultation was performed for reassessment. At the end of the 12-week program (T12), there was a face-to-face medical consultation. At 16 weeks (T16), another re-evaluation teleconsultation was performed.
The control group also had the first medical consultation, in which the patients were instructed in behavioral and lifestyle measures and were prescribed a 12-week PFMT program. However, despite also including domiciliary exercises to be performed three times a day, the PFMT program consisted of only two initial individual face-to-face sessions with the therapist followed by twice-weekly group classes with the same therapist (also divided into 3 phases with the gradual addition of exercises of increasing difficulty in terms of duration, number of repetitions and positions), and all consultations were face-to-face.
The two PMR doctors performed the pelvic floor rehabilitation consultation and the therapist conducted the face-to-face individual, video and class sessions. Patients could contact the therapist at any time for support or questions, and those in the intervention group were also contacted by her every 15 days to check for adherence to the video sessions. The primary outcome of this study was to assess UI-related quality of life using the Portuguese Version of King's Health Questionnaire (KHQ) [14].
The secondary outcome measures were defined as:
-
UI severity using ICS pad testing [11] and the Portuguese version of the International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF [15]), considering 2.5 points a minimal clinically important difference (MCID);
-
global perception of improvement by the patient using the Portuguese version of the Patient Global Impression of Improvement (PGI-I) Scale [16];
-
sexual function using the Portuguese version of the Female Sexual Functioning Index (FSFI) [17];
-
symptoms of depression/anxiety using the Portuguese version of the Hospital Anxiety & Depression Scale (HADS) questionnaire [18];
-
satisfaction and adherence to treatment using the 9-point Likert scale and the number of performed sessions self-reported and reported by the therapist.
Outcomes were measured at baseline (T0) and T12, except for the ICIQ-SF, which was also measured at T16.
KHQ, HADS and FSFI were given to patients to fill out at the end of each consultation in another area of the PMR Department. The remaining questionnaires were applied during consultation.
As a measure of quality, a bladder scan (BS) was performed on each patient at the start of the ICS pad testing at T0 and T12.
The sample size was determined using WinPepi software, version 11.65. Assuming a significance level of 5%, statistical power of 80% and allocation ratio between intervention and control group of 1 to 1, magnitude of difference between the two groups of 10.24 points on KHQ, variability of 10,545 units in the intervention group and 6.23 units in the control group, we estimated that 24 women were needed to address the primary objective, 12 for each group.
Data analyses were performed by another professional who was blinded to the group allocation.
In the following intention-to-treat analyses, all randomized patients were included excepted one from the intervention group who dropped out, as shown in Fig. 1.
Statistical analysis was carried out using SPSS software, version 25.
We used mean (standard deviation) and median (interquartile range) in the characterization of variables with normal or non-normal distribution, respectively. For categorical variables we used proportions. For comparison between groups at T12, for continuous variables, we used the independent-samples Student's t-test for normal distribution and Mann-Whitney test if non-normal distribution was verified. To compare categorical variables, we used a chi-square test or Fisher exact test, as appropriate. A paired-samples t-test was used to test the difference of means in total KHQ and in daily UI pad number between T0 and T12 and in total ICIQ-SF between T0 and T16. A Wilcoxon signed-rank test was used to test the difference of the median ICS pad testing between T0 and T12.
A spaghetti plot was also included, representing the trajectory of each patient and each group at the two or four follow-up time points (at 0 and 12 weeks for the primary outcome and at 0, 6, 12 and 16 weeks for the total ICIQ-SF).
Our study was approved by the National Data Protection Committee and the Portuguese Ethics Committee of São João Hospital University Center (approval no. 114/2021). The trial was registered at www.ClinicalTrials.gov, no. NCT05114395.
Results
A total of 35 women were enrolled, with 18 randomized to intervention and 17 to control.
Of the 23 women excluded from this protocol, the 11 who refused to participate in the study or had a negative ICS pad testing followed the traditional model of PFMT, and the 8 women with pelvic floor muscle strength grade 1 in the MOS had individual PFMT sessions with a specialized therapist. Furthermore, two of the excluded women dropped out of the consultation (1 who could not be contacted and 1 who became pregnant), and two postponed the therapeutic program because of shoulder and knee surgeries. These patients did not show significant differences compared to those included in the study analysis according to the characteristics described in Table 1.
At baseline, the intervention and control groups were similar in terms of sociodemographic and clinical characteristics, as shown in Table 1. The initial mean BS values were also similar between groups (p = 0.072). One participant from the intervention group was lost to follow-up because of contact and scheduling conflicts after the first appointment, so her data were not included in the following analysis of this study. She also dropped out of the consultation. There were no losses to follow-up in the control group.
As shown in Table 2, adherence to behavioral measures was high, with a greater impact at T12 than at T6, highlighting 100% adherence in reducing daily consumption of green and black tea, > 70% when increasing daily physical activity and > 90% in timed voiding every h.
Adherence to PFMT measures at T12, namely to video/class sessions and the domiciliary PFMT program at least once a week, was 100% and > than 50%, respectively. At T6, adherence to video/class sessions at least twice a week was also high, > 80%.
Considering the PGI-I scale, more than half of the patients in each group considered they were better or much better off with their treatment. The median satisfaction at T12 was 9 in 10 in both groups.
Concerning the ICIQ-SF, a MCID was achieved in both groups at T6, T12 and T16. In the control group 11.8% of the patients and in the intervention group 41.2% reported having no urine losses within the last 4 weeks at the 16-week consultation.
Considering the total KHQ mean score, UI-related quality of life significantly improved in both the intervention and control groups between T0 and T12 (p = 0.002 and p < 0.001, respectively), although the magnitude of the improvement was not significantly different between groups (–10.0 vs. –9.5 points, p = 0.918, respectively).
Additionally, in the control and intervention groups a significant reduction of UI severity was objectified by a decrease at T12 in the total ICIQ-SF mean score (–4.9 vs. –5.6 points, p < 0.001 in both groups), ICS pad testing median score (–11.0 vs. –11.9 points, p < 0.001 in both groups) and number of daily UI pads used mean score (–0.6 vs. –1.2 points, p = 0.004 and p = 0.001, respectively). However, there was no significant difference in the intergroup analysis (p = 0.455, p = 0.999 and p = 0.240, respectively). There was also no significant difference in the intergroup analysis in the final mean BS values in either group (p = 0.501). Furthermore, no significant difference was observed between T0 and T12 BS measurements across the entire sample (p = 0.071).
As shown in Table 3, there was also an improvement in sexual function documented by the total FSFI mean and a reduction in the presence of symptoms of depression and anxiety shown by the mean HADS-Depression and HADS-Anxiety, but also with no significant differences between groups (p = 0.417, p = 0.741 and p = 0.081, respectively).
The mean body mass index (BMI) also decreased significantly by 0.6 points in the control and intervention groups (p = 0.002 and p < 0.001, respectively).
The proportion of patients with grades 4 and 5 on the MOS in the intervention group was superior to that in the control group (83.3% vs. 58.8%) at T12, but with no significant difference between groups (p = 0.717 and p = 0.140, respectively).
As Fig. 3 shows, a global trend toward improvement considering the total KHQ and the total ICIQ-SF scores was observed in the time points measured in both groups, in both the individual and group analyses.
a and b: Spaghetti plots showing the trajectory of each patient and each study group at the two or four follow-up time points (at 0 and 12 weeks for the total KHQ and at 0, 6, 12 and 16 weeks for the total ICIQ-SF, respectively). KHQ = King’s Health Questionnaire. ICIQ-SF = International Consultation on Incontinence Questionnaire-Short Form
Discussion
We showed a significant and similar improvement in total KHQ mean score in the UI-related quality of life seen at T12 in the control and the intervention groups as well as a reduction in UI severity shown by a significant reduction in the total KHQ mean score, total ICIQ-SF mean score, ICS pad testing median score and number of daily UI pads used mean score. However, the magnitude of the variation between the baseline and last measurement was not significantly different between the two groups, corroborating the most recent literature [7].
The COVID-19 pandemic gave a boost to using telemedicine and telerehabilitation in the immediate future.
Only a few studies exist in the literature comparing the efficacy of PFMT telerehabilitation programs with the conventional ones. The present study is therefore important as it highlights the potential of using the telerehabilitation interventions, in terms of cost and time savings and pollution prevention.
However, heterogeneities in outcomes of measured and designed protocols can explain the lack of consensus on telehealth PFMT programs.
Our study was similar to that of Sjöström et al. in concluding that an internet-based treatment for SUI is a new, cost-effective treatment, but they compared the modality with treatment information provided by post, analysing different economic indicators [19].
Hui et al. showed that videoconferencing is as effective as conventional methods in the management of UI in an 8-week intervention period with one session per week, but their intervention period was not the one considered by current guidelines to assess sustainable benefits [8].
The results of Carrión Pérez et al.'s pilot study were similar to ours but included only 19 patients in a 12-week program. However, their adherence to treatment between groups was uneven, making the comparison between groups less robust than in our study (100% in the telerehabilitation group vs. 33.3% in the control group) [5].
Contrary to Fitz et al., who observed better adherence to the PFMT only in the first month in the outpatient group, we achieved optimal adherence not only at T6 but also and higher at T12 in the two groups, to both behavioral measures and the PFMT program, highlighting the importance of a mid-program consultation. Moreover, we considered the three individual face-to-face sessions, two at the beginning of the program and one before the last month of the program with higher exercises complexity, as well as the intensive and continuous supervision by telephone contact by the therapist every 2 weeks that we included in our protocol in the intervention group, to be innovative and critical to achieving our determined results, with emphasis on our outstanding adherence [20].
We designed a protocol that included the most possible characteristics with clinical and sociodemographic relevance in our sample, as well as the outcomes known in the literature and adequate for our objective, in the greatest number of time points that we could, seeking to give the highest strength to our design, considering all the RCTs published until now.
The literature reports that weight loss reduces UI severity and, in some instances, cures it [21]. BMI decreased significantly in both groups, and we hypothesized that our protocol design with intensive monitoring that allowed reinforcement of the importance of behavioral measures for the success of the intervention in improving UI could also explain this, as even in pandemic times we also noticed an increase in daily physical activity practice in both groups.
Furthermore, our sample had an average age of 45.5 ± 7.2 years, corroborating the findings of Liu et al., who considered 45–59 the age range where the incidence of SUI peaks in women, and of López et al., who showed the highest prevalence (43.4%) in UI reported by women aged 36–50 years [21, 22].
Nevertheless, since only one loss to follow-up was observed in the intervention group, we did not expect a great effect on the strength of our determined results due to a negligible attrition bias.
Moreover, although we used a methodologically robust and adequately powered RCT to access the effectiveness of a hybrid telerehabilitation protocol, the carry-over effect of this intervention over time was not evaluated, so its long-term benefits are not yet known.
Additionally, the scale-up and adoption of the purposed intervention require the patients to have technological skills, which may be insufficient among elderly patients with UI who may have low digital literacy.
In conclusion, this hybrid telerehabilitation protocol showed effectiveness comparable to the traditional model with respect to improving UI symptoms and UI-related quality of life, proving to be a viable alternative, especially in pandemic times.
We are expanding this study considering that further long-term outcome studies and health economic assessments are required to validate these findings.
References
D'Ancona C, Haylen B, Oelke M, Abranches-Monteiro L, Arnold E, Goldman H, Hamid R, Homma Y, Marcelissen T, Rademakers K, Schizas A, Singla A, Soto I, Tse V, de Wachter S, Herschorn S. The International Continence Society (ICS) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourol Urodyn. 2019;38(2):433–77. https://doi.org/10.1002/nau.23897.
Correia S, Dinis P, Rolo F, Lunet N. Prevalence, treatment and known risk factors of urinary incontinence and overactive bladder in the non-institutionalized Portuguese population. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(12):1481–9. https://doi.org/10.1007/s00192-009-0975-x.
Minassian VA, Drutz HP, Al-Badr A. Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet. 2003;82(3):327–38. https://doi.org/10.1016/s0020-7292(03)00220-0.
Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, Coyne K, Kelleher C, Hampel C, Artibani W, Abrams P. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50(6):1306–14; discussion 1314-1305. https://doi.org/10.1016/j.eururo.2006.09.019.
Carrión Pérez F, Rodríguez Moreno MS, Carnerero Córdoba L, Romero Garrido MC, Quintana Tirado L, García Montes I. Telerehabilitation to treat stress urinary incontinence. Pilot study. Med Clin (Barc). 2015;144(10):445–8. https://doi.org/10.1016/j.medcli.2014.05.036.
Hay-Smith EJ, Lc BB, Hendriks HJ, de Bie RA, van Waalwijk van Doorn ES. Pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst Rev. 2001;(1):Cd001407. https://doi.org/10.1002/14651858.Cd001407.
da Mata KRU, Costa RCM, Carbone ÉDSM, Gimenez MM, Bortolini MAT, Castro RA, Fitz FF. Telehealth in the rehabilitation of female pelvic floor dysfunction: a systematic literature review. Int Urogynecol J. 2021;32(2):249–59. https://doi.org/10.1007/s00192-020-04588-8.
Hui E, Lee PS, Woo J. Management of urinary incontinence in older women using videoconferencing versus conventional management: a randomized controlled trial. J Telemed Telecare. 2006;12(7):343–7. https://doi.org/10.1258/135763306778682413.
Novara G, Checcucci E, Crestani A, Abrate A, Esperto F, Pavan N, De Nunzio C, Galfano A, Giannarini G, Gregori A, Liguori G, Bartoletti R, Porpiglia F, Scarpa RM, Simonato A, Trombetta C, Tubaro A, Ficarra V. Telehealth in urology: a systematic review of the literature. How much can telemedicine be useful during and after the COVID-19 pandemic? Eur Urol. 2020;78(6):786–811. https://doi.org/10.1016/j.eururo.2020.06.025.
Baessler K, Schüssler B. The Effects of Pregnancy and Childbirth on the Pelvic Floor. In: Schüssler B (ed) Pelvic Floor Re-education, 2nd edn. Springer-Verlag, London, United Kingdom; 2008, pp 42-48. https://doi.org/10.1007/978-1-84628-505-9.
Krhut J, Zachoval R, Smith PP, Rosier PF, Valanský L, Martan A, Zvara P. Pad weight testing in the evaluation of urinary incontinence. Neurourol Urodyn. 2014;33(5):507–10. https://doi.org/10.1002/nau.22436.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26. https://doi.org/10.1007/s00192-009-0976-9.
Bø K, Berghmans B, Mørkved S, Van Kampen M, editors. Evidence-based physical therapy for the pelvic floor. Edinburgh: Elsevier; 2015.
Viana R, Viana S, Neto F, Mascarenhas T. Adaptation and validation of the King’s Health Questionnaire in Portuguese women with urinary incontinence. Int Urogynecol J. 2015;26. https://doi.org/10.1007/s00192-015-2628-6
Tamanini JT, Dambros M, D'Ancona CA, Palma PC, Rodrigues Netto N Jr. Validation of the "International Consultation on Incontinence Questionnaire-Short Form" (ICIQ-SF) for Portuguese. Rev Saude Publica. 2004;38(3):438–44. https://doi.org/10.1590/s0034-89102004000300015.
Domingues L, Cruz E (2011) Adaptação Cultural e Contributo para a Validação da Escala Patient Global Impression of Change. Ifisionline. http://www.ifisionline.ips.pt/media/3jan_vol2_n1/pdfs/artigo4_vol2n1.pdf. Accessed 29 Dec 2021.
Pechorro P, Diniz A, Almeida S, Vieira R (2009) Validação portuguesa do índice de Funcionamento Sexual Feminino (FSFI) / Portuguese validation of the Female Sexual Function Index (FSFI). Laboratório de Psicologia 7. http://publicacoes.ispa.pt/index.php/lp/article/download/684/665. Accessed 29 Dec 2021. https://doi.org/10.14417/lp.684
Pais-Ribeiro J, Silva I, Ferreira T, Martins A, Meneses R, Baltar M. Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychol Health Med. 2007;12(2):225–35; quiz 235-227. https://doi.org/10.1080/13548500500524088.
Sjöström M, Umefjord G, Stenlund H, Carlbring P, Andersson G, Samuelsson E. Internet-based treatment of stress urinary incontinence: a randomised controlled study with focus on pelvic floor muscle training. BJU Int. 2013;112(3):362–72. https://doi.org/10.1111/j.1464-410X.2012.11713.x.
Fitz FF, Gimenez MM, de Azevedo FL, Matias MMP, Bortolini MAT, Castro RA. Pelvic floor muscle training for female stress urinary incontinence: a randomised control trial comparing home and outpatient training. Int Urogynecol J. 2020;31(5):989–98. https://doi.org/10.1007/s00192-019-04081-x.
López M, Ortiz AP, Vargas R. Prevalence of urinary incontinence and its association with body mass index among women in Puerto Rico. J Womens Health (Larchmt). 2009;18(10):1607–14. https://doi.org/10.1089/jwh.2008.1207.
Liu L, Zhang Y, Gong J, Chen X, Wu H, Zhu W. Effects of different treatment methods on the clinical and urodynamic state of perimenopausal women with stress urinary incontinence. Iran J Public Health. 2018;47(8):1090–7.
Author information
Authors and Affiliations
Contributions
M Santiago: Protocol application, Data collection, Manuscript writing
P Cardoso-Teixeira: Data collection, Manuscript writing
J Firmino-Machado: Data analysis
S Pereira: Exercise sessions design and conduct, Data collection
S Moreira: Protocol conception, design and application, Data collection, Manuscript editing
Corresponding author
Ethics declarations
Conflict of interests
All authors declare they have no conflict of interests.
Ethical approval
All authors revised and approved the final version of the manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Santiago, M., Cardoso-Teixeira, P., Pereira, S. et al. A Hybrid-Telerehabilitation Versus a Conventional Program for Urinary Incontinence: a Randomized Trial during COVID-19 Pandemic. Int Urogynecol J 34, 717–727 (2023). https://doi.org/10.1007/s00192-022-05108-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05108-6