Abstract
Aims/hypothesis
Type 2 diabetes and non-alcoholic fatty liver disease (NAFLD) are prevalent diseases of metabolic origin. We examined the association between NAFLD and the development of type 2 diabetes among non-Asian adults, and whether the association differs by race.
Methods
We analysed data from the Coronary Artery Risk Development in Young Adults (CARDIA) study, a population-based prospective cohort study. Participants underwent non-contrast abdominal computed tomography (CT) at baseline (2010–2011) and assessment of glucose measures at the follow-up exam (2015–2016). NAFLD was defined as liver attenuation ≤51 Hounsfield units on CT images after exclusion for other liver fat causes. Race was self-reported. We used targeted maximum likelihood estimation (TMLE) with machine-learning algorithms to estimate difference in type 2 diabetes risk between the NAFLD and non-NAFLD groups.
Results
Of the 1995 participants without type 2 diabetes at baseline (mean age±SD, 50.0±3.6 years; 59% women; 55.0% White and 45.0% Black), 21.7% of White and 16.8% of Black participants had NAFLD at baseline, and 3.7% of White and 8.0% of Black participants developed type 2 diabetes at follow up. After multivariable adjustment, risk difference for type 2 diabetes associated with NAFLD vs no NAFLD was 4.1% (95% CI 0.3%, 7.9%) among White participants and −1.9% (95% CI −5.7%, 2.0%) in Black participants.
Conclusions/interpretation
NAFLD was associated with a higher risk of type 2 diabetes among White participants but not among Black participants. This finding suggests that the effect of liver fat on impaired glucose metabolism may be smaller in Black than in White individuals.
Graphical abstract

Similar content being viewed by others

Introduction
Approximately 34.2 million Americans (10.5% of the US population) have diabetes, and 1.5 million Americans are diagnosed with diabetes every year [1]. The prevalence of type 2 diabetes is twofold higher among African American than White individuals [2]. The rising number of individuals with type 2 diabetes and its racial disparity remains challenging.
The liver plays a key role in the control of glucose homeostasis by controlling glycolysis and gluconeogenesis [3]. Non-alcoholic fatty liver disease (NAFLD) is the most common chronic liver disease in the USA [4] and is reported to be associated with type 2 diabetes [5,6,7]. Despite this, African Americans have significantly lower NAFLD prevalence compared with White individuals [8]. Thus, there may be a different relationship between NAFLD and risk of type 2 diabetes by race. However, associations between NAFLD and incident type 2 diabetes have been reported in Asian populations [5,6,7], with few studies in the USA being conducted among individuals of different race. Therefore, it remains uncertain whether NAFLD is associated with incident type 2 diabetes among non-Asian populations and whether the association differs by race.
Prior studies investigating the association between NAFLD and incident diabetes have a major limitation. In these studies, the NAFLD group had dissimilar baseline characteristics compared with the non-NAFLD group (e.g., adiposity, insulin resistance and behavioural characteristics) [5,6,7]. Furthermore, there are many shared metabolic risk factors between type 2 diabetes and NAFLD which facilitate model misspecification and biased estimates of exposure effect. In this setting, implementation of targeted maximum likelihood estimation (TMLE) using machine-learning algorithms with a rich set of potential confounders can be advantageous [9]. It improves the chances of correct model specification since TMLE is a doubly robust method if either exposure or outcome mechanisms are estimated consistently; and TMLE allows for flexible and data-adaptive estimation using non-parametric machine-learning methods (particularly ensemble methods, such as SuperLearner) to avoid strong assumptions about the distribution of the data (e.g., multivariate normality). In addition, it allows us to prevent overfitting even when adjusting for a variety of covariates. Thus, it may be preferable to misspecified regressions (e.g., generalised linear regression) to generate less biased estimates [9, 10].
The Coronary Artery Risk Development in Young Adults (CARDIA) study is a prospective longitudinal cohort study among White and Black participants who underwent non-contrast computed tomography (CT) scanning of the abdomen and assessments of glucose measures between 2010 and 2011 [11]. Among the CARDIA participants free of diabetes, we assessed whether CT-defined NAFLD was associated with incident type 2 diabetes and whether the association differed by self-reported race. We used TMLE with machine-learning algorithms to estimate difference in type 2 diabetes risk between the NAFLD and non-NAFLD groups.
Methods
Study population
The CARDIA study is an ongoing longitudinal cohort study that enrolled 5115 Black and White participants, aged 18 to 30 years, from four US field centres (Birmingham [AL], Chicago [IL], Minneapolis [MN] and Oakland [CA]) in 1985 and 1986 [11]. CARDIA follow-up exams were conducted 2, 5, 7, 10, 15, 20, 25 and 30 years after CARDIA baseline measures. All participants provided written informed consent at each study visit, and institutional review boards at each field centre and the coordinating centre approved the study annually. The current analysis was restricted to the 3498 CARDIA participants who attended the 25 year follow-up exam (our ‘baseline’ for longitudinal analysis) between 2010 and 2011 and the 30 year follow-up exam (our ‘follow up’ for longitudinal analysis) between 2015 and 2016. For the current analyses, we excluded: (1) participants who did not undergo CT scanning of the abdomen due to pregnancy or severe obesity (weighing more than 450 lbs); (2) participants with missing CT measurements for liver attenuation; (3) participants who had chronic liver disease or secondary hepatic steatosis (i.e. self-reported hepatitis or cirrhosis, hepatitis C, hepatitis B, primary biliary cholangitis, and hemochromatosis); (4) men who consumed ≥30 g alcohol per day and women who consumed ≥20 g alcohol per day [12]; (5) participants with self-reported HIV; (6) participants taking medications that cause hepatic steatosis (e.g., amiodarone, diltiazem, methotrexate, tamoxifen, valproic acid and/or steroids); and (7) participants with missing data for glucose measurements at baseline or follow up, and participants with diabetes already present at baseline (Fig. 1).
Quantitative detection methods of liver fat content
Non-contrast CT scans were performed at baseline using GE multidetector CT scanners (GE 750HD 64 [Birmingham centre] or GE LightSpeed VCT 64 [Oakland centre]; GE Healthcare, Waukesha, WI, USA) or a Siemens multidetector CT scanner (Sensation 64 [Chicago and Minneapolis centres]; Siemens Medical Solutions, Erlangen, Germany) [13]. Image analysis and quality control were performed at a core reading centre (Wake Forest University Health Sciences, Winston-Salem, NC, USA). Liver attenuation was measured in the right lobe of the liver using CT slices through the upper abdomen. Liver attenuation was calculated as the mean of nine measurements from three CT slices (three measurements per slide) using circular regions of interest of 2.6 cm2. The interclass correlation coefficient between different readers on a random selected sample of 156 participants was 0.975 for liver attenuation measured by CT [13].
NAFLD was defined as liver attenuation measured by CT ≤51 Hounsfield units (HU) (which corresponds to a liver:spleen attenuation ratio <1 [14, 15]), without other causes of liver fat being present.
Glucose, race and other baseline characteristics
Fasting glucose was determined in participants who reported fasting for ≥8 h when blood was drawn by venepuncture according to a standard protocol [11]. Fasting glucose was measured using hexokinase coupled to glucose 6-phosphate dehydrogenase, manufactured by Linco Research (St Louis, MO, USA). Using a commercially purchased pool of control samples, quality control was conducted; within-run precision (%CV) was <1% and the between-run precision (%CV) was <2%. Prevalent diabetes was defined as fasting glucose ≥7.0 mmol/l or the use of diabetes medications at baseline. Incident type 2 diabetes was defined as fasting glucose ≥7.0 mmol/l or the use of diabetes medications at follow up among those without prevalent diabetes at baseline [16].
Other data were collected using standardised protocols and quality control procedures across study centres at each visit, as described previously (see electronic supplementary material [ESM] Methods for full details) [11]. These included age, sex, socioeconomic status (education attainment, income, marital status, employment status), behavioural characteristics (smoking, alcohol consumption, sugar-sweetened carbonated drink consumption, physical activity), medical history (history of coronary heart disease, stroke and bariatric surgery, family history of diabetes, and use of antihyperglycaemic, antihypertensive or lipid-lowering medications), physical measurements (BP, BMI, waist circumference, waist-to-hip ratio), fasting laboratory measurements (insulin [including HOMA-IR], total cholesterol, triglyceride, HDL-cholesterol, LDL-cholesterol, eGFR, high-sensitivity C-reactive protein [hs-CRP]) and CT-derived fat measures (total abdominal fat volume, subcutaneous adipose tissue and visceral adipose tissue). The race of each participant was self-assigned at the CARDIA study baseline according to the following given categories:: ‘Hispanic’, ‘Black, not Hispanic’, ‘White, not Hispanic’, ‘American Indian or Alaskan native’, ‘Asian or Pacific Islander’, ‘Don’t Know’ or ‘No Answer’. Race was confirmed by the participants of the CARDIA study at the 2 year follow up. Here, we include self-reported race as a proxy for the social determinants of health that are associated with disparities in morbidity and mortality [17,18,19].
Statistical analyses
Summary statistics for baseline characteristics of participants were calculated overall, and for non-NAFLD and NAFLD groups, separately. The statistical significance of differences between the groups was determined using the unpaired t test or Mann–Whitney U test for continuous variables, and χ2 tests for categorical variables. Assuming that missing data for covariates occurred independently of missing glucose measures, all variables with missing data (ESM Table 1) were imputed with 20 data sets using chained equations [20]. Results from each imputed dataset were combined using the standard rules from Rubin [21].
The 5 year cumulative incidence of type 2 diabetes was calculated separately in the non-NAFLD and NAFLD groups at baseline. Risk difference and relative risk for incident type 2 diabetes associated with NAFLD were calculated in unadjusted and adjusted models. We used the TMLE model, a semiparametric doubly robust method, which provides an efficient substitution estimator [9]. The implementation of TMLE involves the following steps: (1) generating estimators for the outcome model on exposure and all potential confounders (i.e. probability of having type 2 diabetes calculated using NAFLD and covariates [outcome regression]); (2) generating estimators for the exposure model on all potential confounders (i.e. probability of having NAFLD calculated using covariates [propensity score regression]); (3) calculating the clever covariate based on the exposure model for both exposed and unexposed groups; (4) fluctuating the initial estimator of the outcome model to target the parameter of interest; and (5) calculating the risk of outcome of interests for exposed and unexposed groups, and then calculating the measure of association of interest [22]. We used the SuperLearner algorithm to estimate both propensity score regression and outcome regression. The SuperLearner algorithm combines a library of data-adaptive machine-learning models and parametric models (i.e. ensemble method) in order to calculate an estimator that may perform better than any single model in the library (see ESM Methods for details) [23]. This approach minimises bias and overfitting compared with using misspecified regressions (e.g., linear associations). Therefore, we adjusted for a rich set of covariates.
Covariates included sex, age, self-reported race (not used in race-stratified analyses), study site, socioeconomic status (education attainment, income, marital status and employment status), behavioural characteristics (smoking status, alcohol consumption, sugar-sweetened carbonated drink consumption and physical activity score) and clinical characteristics at baseline, including BMI, waist circumference, waist-to-hip ratio, hypertension, history of coronary heart disease, history of stroke, history of bariatric surgery, family history of type 2 diabetes, fasting glucose, total cholesterol, triglycerides, HDL-cholesterol, LDL-cholesterol [24], HOMA-IR [25], hs-CRP, eGFR [26], measures of abdominal fat (i.e. total abdominal fat volume, subcutaneous adipose tissue and visceral adipose tissue) and use of lipid-lowering drugs. Covariates were selected a priori because they have been associated with NAFLD and type 2 diabetes [5, 6, 27,28,29,30]. We tested for heterogeneity in the association between NAFLD and incident type 2 diabetes by self-reported race using the TMLE marginal structural model [31].
Mediation analyses were performed, given that the following covariates can be mediators of the associations between NAFLD and incident type 2 diabetes: baseline fasting glucose, HOMA-IR and hs-CRP. Structural equation modelling was used with the Lavaan package [32]. Total, direct and indirect effect estimates were calculated using multivariable adjusted linear regression analysis, adjusted for the same potential confounding variables.
To compare NAFLD severity and other factors by self-reported race, we conducted an exploratory analysis among participants with NAFLD. In sensitivity analyses, we conducted the following: (1) multivariable linear regression and multivariable Poisson regression analyses to compare results obtained using TMLE; (2) multivariable linear and Poisson regression analyses using liver attenuation measured by CT as a continuous variable; (3) generalised additive models to validate the threshold of liver attenuation measured by CT for NAFLD affecting incident type 2 diabetes; (4) analyses without imputing missing covariates; and (5) analyses excluding individuals with impaired fasting glucose (fasting glucose levels ≥5.6 mmol/l to <7.0 mmol/l) at baseline in addition to prevalent diabetes.
Statistical analyses were performed using R for Windows, version 3.6.0 (R Foundation for Statistical Computing, Vienna, Austria). Statistical significance was defined by a two-sided p value <0.05. For interpretation of statistical interactions, we used p<0.05.
Results
Of the 3498 participants (56.6% women and 46.9% Black participants) who attended the baseline exam, we excluded 1503 participants (Fig. 1), for a final analysis sample of 1995 individuals (mean age±SD 50.0±3.6 years, 58.8% female, 55.0% White and 45.0% Black participants). Overall demographic and clinical characteristics of the included participants, and characteristics by the presence or absence of NAFLD are shown in Table 1. Compared with those without NAFLD, participants with NAFLD were more likely to be male, White, and have higher BMI, waist circumference, fasting glucose, HOMA-IR, serum triglyceride levels, hs-CRP levels, subcutaneous adipose tissue volume and visceral adipose tissue volume. ESM Table 2 shows the characteristics of participants according to race and NAFLD. Compared with those without NAFLD, among White participants, those with NAFLD were more likely to consume >1 sugar-sweetened carbonated drink per day and partake in less physical activity per week, while among Black participants, those with NAFLD were more likely to smoke (ESM Table 2).
Of the 1995 participants, 5.7% (n=113) had developed type 2 diabetes at the 5 year follow-up exam (Table 2). In an unadjusted model, risk difference and relative risk for type 2 diabetes at follow up associated with NAFLD at baseline were 7.97% (95% CI 5.44%, 10.51%) and 2.94 (95% CI 2.02, 4.27), respectively. Adjusted risk difference and relative risk for type 2 diabetes associated with NAFLD were 0.87% (95% CI −1.33%, 3.06%) and 1.16 (0.81, 1.68), respectively. The weighted algorithms chosen by SuperLearner show each coefficient (weight) of several statistical or machine-learning models to build the final ensemble algorithms (ESM Table 3).
The TMLE marginal structural model showed that self-reported race modified the association of NAFLD with incident type 2 diabetes (p for interaction <0.001). In the stratified analysis by self-reported race, 21.7% (n=238) of White and 16.8% (n=151) of Black participants had NAFLD at baseline, and 3.7% (n=41) of White and 8.0% (n=72) of Black participants had developed type 2 diabetes at follow up (Table 2). In total, 1.6% of participants without NAFLD and 11.3% of participants with NAFLD had developed type 2 diabetes among White people, while among Black participants 7.0% of those without NAFLD and 13.2% of those with NAFLD had developed type 2 diabetes at follow up. Adjusted risk difference for type 2 diabetes associated with NAFLD was 4.10% (95% CI 0.27%, 7.92%) among White participants and −1.85% (95% CI −5.68%, 1.99%) among Black participants. The relative risk for the association between NAFLD and incident type 2 diabetes was 2.84 (95% CI 1.42, 5.69) among White participants and 0.79 (95% CI 0.46, 1.34) among Black participants. The weighted algorithms chosen by SuperLearner are shown in ESM Table 3.
Exploratory analysis
Among participants with NAFLD, liver attenuation was lower in White participants (38.9±11.0 HU) than Black participants (42.3±9.5 HU), with a p value of 0.002 (ESM Table 2). Among participants with NAFLD, waist-to-hip ratio and visceral adipose tissue volume were higher among White participants than Black participants (p value <0.001 for both), while BMI (p=0.001) and subcutaneous adipose tissue volume (p<0.001) were lower (ESM Table 2). Among participants with NAFLD, fasting insulin levels and HOMA-IR at baseline were higher in Black participants than White participants, with p values of 0.007 and 0.010, respectively (ESM Table 2).
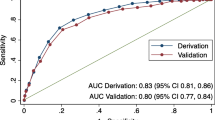
Sensitivity analyses
Results were similar when we used multivariable linear regression and Poisson regression models instead of the TMLE (ESM Table 4), and when we used liver attenuation measured by CT as a continuous variable instead of using a cut-off value of ≤51 HU for NAFLD (ESM Table 5). Figure 2, generated using generalised additive models, shows the appropriateness of using a liver attenuation cut-off value of ≤51 HU to define NAFLD and assess its impact on incident type 2 diabetes, and the higher impact of liver lipid storage on type 2 diabetes among White vs Black participants. ESM Table 6 shows the characteristics of the participants without imputed missing covariates. Results with and without imputed missing covariates were similar (ESM Table 7). ESM Table 8 shows the results excluding individuals with impaired fasting glucose at baseline. These results were similar to the results including participants with impaired fasting glucose.
Cumulative probability of type 2 diabetes at follow up (2015–2016) associated with liver attenuation measured by CT at baseline (2010–2011) (n=1995). The black dotted line indicates the liver attenuation cut-off value used in the study (51 HU). Cumulative probabilities of type 2 diabetes were calculated using generalised additive models
Mediation analyses
In mediation analyses among White participants, the direct effect of NAFLD (z) (adjusted risk difference: 5.80% [95% CI 2.63%, 8.97%]) accounted for most of the total effect (z+a1b1+a2b2+a3b3, whereby a1b1, a2b2, and a3b3 represent the indirect effect of NAFLD on type 2 diabetes through fasting glucose, HOMA-IR and hs-CRP, respectively; adjusted risk difference: 6.63% [95% CI 3.40%, 9.86%]) on type 2 diabetes risk (Fig. 3 and ESM Table 9). HOMA-IR at baseline significantly mediated the association between NAFLD and incident type 2 diabetes (a2b2; adjusted risk difference 0.97% [95% CI 0.36%, 1.58%]), while fasting glucose (a1b1) and hs-CRP (a3b3) did not (ESM Table 9). Among Black participants, neither the total (z+a1b1+a2b2+a3b3) nor direct (z) effect of NAFLD was significantly associated with the incident type 2 diabetes, with adjusted risk differences of 0.17% (95% CI −4.96%, 5.30%) and −1.50% (95% CI −6.62%, 3.62%), respectively.
Path model diagram with the results of mediation analysis using structural equation modelling in (a) n=1098 White participants and (b) n=897 Black participants. The path model shows the effect of NAFLD on type 2 diabetes incidence as mediated simultaneously by fasting glucose, HOMA-IR and hs-CRP at baseline. The direction of the path analysis from NAFLD to type 2 diabetes incidence was prespecified. NAFLD was defined as liver attenuation measured by CT ≤51 HU at baseline (2010–2011), which corresponds to a liver:spleen attenuation ratio <1, without other causes of liver fat. Diabetes was defined as fasting glucose ≥7.0 mmol/l or the use of diabetes medications at follow up (2015–2016). We used structural equation modelling. The model adjusted for sex, age, study site, baseline socioeconomic status (education attainment, income, marital status and employment status), baseline behavioural characteristics (smoking status, alcohol consumption, sugar-sweetened carbonated drink consumption and physical activity score) and baseline clinical characteristics, including BMI, waist circumference, waist-to-hip ratio, hypertension, history of coronary heart disease, history of stroke, history of bariatric surgery, family history of diabetes, total cholesterol, triglycerides, HDL-cholesterol, LDL-cholesterol, eGFR, measures of abdominal fat (i.e., total abdominal fat volume, subcutaneous adipose tissue and visceral adipose tissue) and use lipid-lowering drugs. Effect sizes (95% CI) are shown; significant values are displayed in bold
Discussion
In this longitudinal study of a community-based cohort, among participants without diabetes at a mean age of 50.0±3.6 years, NAFLD was more prevalent (21.7% vs 16.8%) and more severe in White participants than in Black participants (liver attenuation measured by CT among participants with NAFLD: 38.9±11.0 vs 42.3±9.5). At the follow-up exam conducted 5 years after baseline, Black participants were more likely to have developed type 2 diabetes than White participants (8.0% vs 3.7%). Using TMLE with machine-learning algorithms, we found that NAFLD at baseline was associated with a higher absolute and relative risk for the development of type 2 diabetes in White participants but not in Black participants. The association observed in White participants was independent of a variety of socioeconomic, behavioural and clinical characteristics, including visceral adipose tissue, insulin resistance and inflammation (using hs-CRP).
In the Framingham Heart Study (mean age±SD 45±6 years; 46% women), which included 1051 White participants without fatty liver at baseline, greater liver fat (defined as lower liver-phantom ratio on abdominal CT) was associated with an increased risk for incident type 2 diabetes over 6 years of follow up [28]. The study did not exclude people with chronic liver disease or secondary hepatic steatosis unless it was caused by excessive alcohol intake at baseline. Furthermore, adjustment for covariates in this study might have been insufficient (e.g., parameters of socioeconomic status, inflammation and insulin resistance were not adjusted for). In the Multi-Ethnic Study of Atherosclerosis (n=3153; median age [IQR] 59 [51–68] years; 39.2% White individuals, 27.1% African American, 21.2% Hispanic and 12.5% Asian), participants with NAFLD had a higher risk for developing diabetes over 9 years of follow up [33]. However, how the association between NAFLD and type 2 diabetes differs by race was not clarified. The current study extends prior knowledge using a larger sample of Black participants and demonstrates that NAFLD was associated with a higher risk for the development of type 2 diabetes in White participants but not in Black participants, independent of a rich set of covariates, including parameters of inflammation and insulin resistance. Furthermore, some of the covariates used in the Multi-Ethnic Study of Atherosclerosis and in the current study can be mediators of the associations between prevalent NAFLD and incident type 2 diabetes (specifically fasting glucose, HOMA-IR and hs-CRP). Thus, we performed mediation analyses. The results indicated that NAFLD was largely directly associated with incident type 2 diabetes among White participants, while HOMA-IR at baseline slightly mediated the association.
Ectopic fat storage, the accumulation of lipid droplets in nonadipose tissues (e.g., the liver, skeletal muscle and pancreas), is associated with insulin resistance and diabetes. Although African Americans have been shown to be at higher risk for type 2 diabetes compared with White individuals, they are likely to have lower levels of ectopic fat [34]. African Americans had lower NAFLD prevalence and severity compared with White adults in a prior study [8], which is consistent with our results. A previous cross-sectional study suggested that Black West African individuals have lower levels of liver fat than Europeans, and greater liver fat was associated with lower insulin sensitivity only in Europeans [35]. We observed that NAFLD was associated with the development of type 2 diabetes only in White adults. These results suggest that fat accumulation in the liver may play less of a role in the development of type 2 diabetes among Black populations.
TMLE with machine-learning algorithms can be preferable to the conventional regression approaches when analysing the current observational data with a large number of variables and potentially complex relationships between them, as it can help protect against bias. The correct model specification is crucial to obtain unbiased estimates. When the exposure groups are dissimilar, as in the current study, careful statistical adjustment for confounders is necessary. There are two broad approaches for confounding adjustment: conventional outcome regression modelling and exposure modelling (propensity score methods). Conventional outcome regression models (e.g., the generalised linear model) can be biased under misspecification of a parametric outcome model [36]. Propensity score methods, on the other hand, require the correct specification of an exposure model. Contrastingly, the TMLE model is a doubly robust method, combining outcome and exposure models to generate an unbiased estimate as long as at least one of the models is correctly specified [9]. TMLE also enables the utilisation of non-parametric machine-learning approaches, which can mitigate model misspecification. We used the ensemble machine learning algorithm, SuperLearner, that combines multiple machine-learning models and uses them to make a prediction as good as or better than any single model. It can empirically identify interactions and nonlinear relationships among variables. It can, therefore, avoid making strong assumptions about the distribution of the data (e.g., multivariate normality) and about the associations between variables (e.g., linear relation). Prior studies showed that TMLE with machine-learning algorithms provided a less biased estimate compared with various other statistical methods [9, 37]. Thus, this method may be preferable for the current cohort data, which has complex relationships between a large number of variables.
The bi-directional relationship between NAFLD and type 2 diabetes has been shown in other studies, even by use of Mendelian randomisation methods [38, 39]. Mendelian randomisation is an epidemiological approach aimed at strengthening causal inference, utilising genetic variants as instrumental variables [40]. It carries a merit of diminishing reverse causality. There have been several studies examining the association between NAFLD and type 2 diabetes using Mendelian randomisation. Liu et al suggested that genetically driven NAFLD significantly increased the risk of type 2 diabetes, while genetically driven type 2 diabetes increased NAFLD risk [38]. Yuan et al also provided evidence that genetic predisposition to type 2 diabetes was associated with an increased risk of NAFLD [39]. Thus, our observational association might be driven by reverse causation, although this is unlikely due to this being a 5 year prospective cohort study. These prior studies, however, involved only European descendants [38, 39]. By using cohort data that included a large number of Black individuals from the USA, the current study was able to suggest racial differences in the association between NAFLD and the risk of type 2 diabetes.
Strengths and limitations
Strengths of this study include the large, well-characterised, community-based cohort of White and Black participants, with high retention and standardised data-collection protocols with quality control. The large sample size of Black participants allowed us to assess associations of NAFLD with type 2 diabetes in White and Black individuals. Additionally, we implemented TMLE using machine-learning algorithms, which enabled adjustments for a rich set of covariates. However, this study has several limitations. First, abdominal CT scans are a less accurate assessment of liver fat that have been outperformed by dual-gradient echo magnetic resonance imaging and proton magnetic resonance spectroscopy [14, 41, 42]. In the current study, among participants with or without prevalent diabetes at baseline (mean age 50.1±3.6 years; 58.1% women; mean BMI 30.4±7.2 kg/m2), the prevalence of NAFLD was 21.8% (227 individuals out of 1041) among Black participants, 24.2% (280 individuals out of 1158) among White participants and 23.1% (507 individuals out of 2199) overall. These values might be relatively lower than the prevalence observed in other studies using ultrasonography or magnetic resonance-based methods [8]. Thus, defining NAFLD by CT scanning might lead to misclassification of NAFLD, and NAFLD-defined by magnetic resonance-based methods might indicate different associations from those observed in the current study. Second, we defined NAFLD as liver attenuation measured by CT ≤51 HU. Although this cut-off value has been used in prior studies [43,44,45], this may be an arbitrary classification. Therefore, in a sensitivity analysis, we used liver attenuation measured by CT as a continuous variable; we found that results were similar (see ESM Table 5). Furthermore, generalised additive models were used to demonstrate the validity of the threshold for incident type 2 diabetes (Fig. 2). Third, diabetes ascertainment included only fasting glucose levels and the use of diabetes medications, but not measures of HbA1c or glucose tolerance testing since data from the CARDIA study does not involve the latter measures at follow up (2015–2016). This could lead to measurement bias. Further studies on associations between NAFLD and incident type 2 diabetes in which diabetes is diagnosed by all of the variables listed above are warranted since none of the prior studies conducted in the USA have been able to achieve this [28, 33]. Fourth, in the CARDIA study, simultaneous assessment of liver chemistry was not carried out alongside CT scans and, thus, we were unable to assess more severe forms of NAFLD (e.g., non-alcoholic steatohepatitis [NASH], which is strongly associated with type 2 diabetes) [46]. Fifth, we used self-reported race as a social construct, not as a genetic construct, in order to focus on the racial disparities in disease based on social determinants of health. To explore the difference in genetic ancestry, further research is needed using genetic/genomic data. Finally, differential attrition by race may have had an impact on our results as a greater percentage of Black participants enrolled in the CARDIA study were excluded from the analysis as compared with White participants.
Conclusions
NAFLD was associated with a higher risk for the development of type 2 diabetes in White participants but not in Black participants. This finding suggests that the effect of liver fat on impaired glucose metabolism may be smaller in Black than in White individuals.
Data availability
Data from the CARDIA study may be requested from the CARDIA coordinating centre. See www.cardia.dopm.uab.edu/ for information.
Abbreviations
- CARDIA:
-
Coronary Artery Risk Development in Young Adults
- CT:
-
Computed tomography
- hs-CRP:
-
High-sensitivity C-reactive protein
- HU:
-
Hounsfield units
- NAFLD:
-
Non-alcoholic fatty liver disease
- TMLE:
-
Targeted maximum likelihood estimation
References
Centers for Disease and Control Prevention (2022) National Diabetes Statistics Report. Available from: www.cdc.gov/diabetes/data/statistics/statistics-report.html. Accessed: 7 January 2023
Menke A, Casagrande S, Geiss L, Cowie CC (2015) Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA 314(10):1021–1029. https://doi.org/10.1001/jama.2015.10029
Han HS, Kang G, Kim JS, Choi BH, Koo SH (2016) Regulation of glucose metabolism from a liver-centric perspective. Exp Mol Med 48:e218. https://doi.org/10.1038/emm.2015.122
Rinella ME (2015) Nonalcoholic fatty liver disease: a systematic review. JAMA 313(22):2263–2273. https://doi.org/10.1001/jama.2015.5370
Sung KC, Jeong WS, Wild SH, Byrne CD (2012) Combined influence of insulin resistance, overweight/obesity, and fatty liver as risk factors for type 2 diabetes. Diabetes Care 35(4):717–722. https://doi.org/10.2337/dc11-1853
Park SK, Seo MH, Shin HC, Ryoo JH (2013) Clinical availability of nonalcoholic fatty liver disease as an early predictor of type 2 diabetes mellitus in Korean men: 5-year prospective cohort study. Hepatology 57(4):1378–1383. https://doi.org/10.1002/hep.26183
Chang Y, Jung HS, Yun KE, Cho J, Cho YK, Ryu S (2013) Cohort study of non-alcoholic fatty liver disease, NAFLD fibrosis score, and the risk of incident diabetes in a Korean population. Am J Gastroenterol 108(12):1861–1868. https://doi.org/10.1038/ajg.2013.349
Rich NE, Oji S, Mufti AR et al (2018) Racial and ethnic disparities in nonalcoholic fatty liver disease prevalence, severity, and outcomes in the United States: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 16(2):198–210.e192. https://doi.org/10.1016/j.cgh.2017.09.041
van der Laan MJ, Rose S (2011) Targeted learning: causal inference for observational and experimental data. Springer, New York
Schuler MS, Rose S (2017) Targeted maximum likelihood estimation for causal inference in observational studies. Am J Epidemiol 185(1):65–73. https://doi.org/10.1093/aje/kww165
Friedman GD, Cutter GR, Donahue RP et al (1988) CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol 41(11):1105–1116. https://doi.org/10.1016/0895-4356(88)90080-7
Chalasani N, Younossi Z, Lavine JE et al (2018) The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology 67(1):328–357. https://doi.org/10.1002/hep.29367
VanWagner LB, Wilcox JE, Colangelo LA et al (2015) Association of nonalcoholic fatty liver disease with subclinical myocardial remodeling and dysfunction: A population-based study. Hepatology 62(3):773–783. https://doi.org/10.1002/hep.27869
Kodama Y, Ng CS, Wu TT et al (2007) Comparison of CT methods for determining the fat content of the liver. AJR Am J Roentgenol 188(5):1307–1312. https://doi.org/10.2214/ajr.06.0992
Piekarski J, Goldberg HI, Royal SA, Axel L, Moss AA (1980) Difference between liver and spleen CT numbers in the normal adult: its usefulness in predicting the presence of diffuse liver disease. Radiology 137(3):727–729. https://doi.org/10.1148/radiology.137.3.6934563
Bancks MP, Kershaw K, Carson AP, Gordon-Larsen P, Schreiner PJ, Carnethon MR (2017) Association of modifiable risk factors in young adulthood with racial disparity in incident type 2 diabetes during middle adulthood. JAMA 318(24):2457–2465. https://doi.org/10.1001/jama.2017.19546
Cunningham TJ, Croft JB, Liu Y, Lu H, Eke PI, Giles WH (2017) Vital signs: racial disparities in age-specific mortality among Blacks or African Americans - United States, 1999-2015. MMWR 66(17):444–456. https://doi.org/10.15585/mmwr.mm6617e1
Singh GK, Daus GP, Allender M et al (2017) Social determinants of health in the United States: addressing major health inequality trends for the nation, 1935-2016. Int J MCH AIDS 6(2):139–164. https://doi.org/10.21106/ijma.236
Benjamins MR, Silva A, Saiyed NS, De Maio FG (2021) Comparison of all-cause mortality rates and inequities between Black and White populations across the 30 most populous US cities. JAMA Netw Open 4(1):e2032086. https://doi.org/10.1001/jamanetworkopen.2020.32086
Sterne JA, White IR, Carlin JB et al (2009) Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 338:b2393. https://doi.org/10.1136/bmj.b2393
Rubin DB (2004) Multiple imputation for nonresponse in surveys. Wiley-Interscience, New York, NY
Petersen ML, van der Laan MJ (2014) Causal models and learning from data: integrating causal modeling and statistical estimation. Epidemiology 25(3):418–426. https://doi.org/10.1097/ede.0000000000000078
van der Laan MJ, Polley EC, Hubbard AE (2007) Super learner. Stat Appl Genet Mol Biol 6:Article25. https://doi.org/10.2202/1544-6115.1309
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18(6):499–502
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419. https://doi.org/10.1007/bf00280883
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Mantovani A, Byrne CD, Bonora E, Targher G (2018) Nonalcoholic fatty liver disease and risk of incident type 2 diabetes: a meta-analysis. Diabetes Care 41(2):372–382. https://doi.org/10.2337/dc17-1902
Ma J, Hwang SJ, Pedley A et al (2017) Bi-directional analysis between fatty liver and cardiovascular disease risk factors. J Hepatol 66(2):390–397. https://doi.org/10.1016/j.jhep.2016.09.022
Younossi Z, Anstee QM, Marietti M et al (2018) Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol 15(1):11–20. https://doi.org/10.1038/nrgastro.2017.109
Weisman A, Fazli GS, Johns A, Booth GL (2018) Evolving trends in the epidemiology, risk factors, and prevention of type 2 diabetes: a review. Can J Cardiol 34(5):552–564. https://doi.org/10.1016/j.cjca.2018.03.002
Rosenblum M, van der Laan MJ (2010) Targeted maximum likelihood estimation of the parameter of a marginal structural model. Int J Biostatistics 6(2):Article 19. https://doi.org/10.2202/1557-4679.1238
Rosseel Y (2012) lavaan: an R package for structural equation modeling. J Stat Softw 48(2):1–36. https://doi.org/10.18637/jss.v048.i02
Shah RV, Allison MA, Lima JA et al (2015) Liver fat, statin use, and incident diabetes: The multi-ethnic study of atherosclerosis. Atherosclerosis 242(1):211–217. https://doi.org/10.1016/j.atherosclerosis.2015.07.018
Alderete TL, Toledo-Corral CM, Goran MI (2014) Metabolic basis of ethnic differences in diabetes risk in overweight and obese youth. Curr Diab Rep 14(2):455. https://doi.org/10.1007/s11892-013-0455-z
Hakim O, Bello O, Ladwa M et al (2019) Ethnic differences in hepatic, pancreatic, muscular and visceral fat deposition in healthy men of white European and black west African ethnicity. Diabetes Res Clin Pract 156:107866. https://doi.org/10.1016/j.diabres.2019.107866
Rao P (1971) Some notes on misspecification in multiple regressions. Am Stat 25(5):37–39. https://doi.org/10.2307/2686082
Neugebauer R, Laan M (2005) Why prefer double robust estimators in causal inference? J Stat Plan Inference 129:405–426. https://doi.org/10.1016/j.jspi.2004.06.060
Liu Z, Zhang Y, Graham S et al (2020) Causal relationships between NAFLD, T2D and obesity have implications for disease subphenotyping. J Hepatol 73(2):263–276. https://doi.org/10.1016/j.jhep.2020.03.006
Yuan S, Chen J, Li X et al (2022) Lifestyle and metabolic factors for nonalcoholic fatty liver disease: Mendelian randomization study. Eur J Epidemiol 37(7):723–733. https://doi.org/10.1007/s10654-022-00868-3
Burgess S, Davey Smith G, Davies NM et al (2019) Guidelines for performing Mendelian randomization investigations. Wellcome Open Res 4:186. https://doi.org/10.12688/wellcomeopenres.15555.2
Musso G, Gambino R, Cassader M, Pagano G (2011) Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med 43(8):617–649. https://doi.org/10.3109/07853890.2010.518623
Lee SS, Park SH, Kim HJ et al (2010) Non-invasive assessment of hepatic steatosis: prospective comparison of the accuracy of imaging examinations. J Hepatol 52(4):579–585. https://doi.org/10.1016/j.jhep.2010.01.008
Cleveland ER, Ning H, Vos MB et al (2019) Low awareness of nonalcoholic fatty liver disease in a population-based cohort sample: the CARDIA study. J Gen Intern Med 34(12):2772–2778. https://doi.org/10.1007/s11606-019-05340-9
VanWagner LB, Ning H, Allen NB et al (2017) Alcohol use and cardiovascular disease risk in patients with nonalcoholic fatty liver disease. Gastroenterology 153(5):1260–1272.e1263. https://doi.org/10.1053/j.gastro.2017.08.012
VanWagner LB, Terry JG, Chow LS et al (2017) Nonalcoholic fatty liver disease and measures of early brain health in middle-aged adults: the CARDIA study. Obesity 25(3):642–651. https://doi.org/10.1002/oby.21767
Gastaldelli A, Cusi K (2019) From NASH to diabetes and from diabetes to NASH: Mechanisms and treatment options. JHEP Rep 1(4):312–328. https://doi.org/10.1016/j.jhepr.2019.07.002
Acknowledgements
This manuscript has been reviewed by the CARDIA Study Presentation and Publications committee for scientific content.
Authors’ relationships and activities
LBVW is a consultant and receives investigator-initiated grant support from W.L. Gore & Associates for unrelated work. APC has received investigator-initiated support from Amgen, Inc. for unrelated work. All other authors declare that there are no relationships and activities that might bias, or be perceived to bias, their work.
Contribution statement
YH and YY were responsible for study conception and design. YH, DML-J and YY collected the data. YH performed the data analysis. YH, LBVW, MRC, MPB, APC, DML-J, TØ and AJV performed the data interpretation. YH, LBVW and YY drafted the manuscript. LBVW, MRC, MPB, APC, DML-J, TØ and AJV critically reviewed and revised the manuscript for important intellectual content. All authors approved the final version of the manuscript to be published. YH is responsible for the integrity of the work as a whole.
Funding
The CARDIA Study is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201800005I and HHSN268201800007I), Northwestern University (HHSN268201800003I), the University of Minnesota (HHSN268201800006I) and the Kaiser Foundation Research Institute (HHSN268201800004I). YY is supported by a grant (no. P20GM104357) from the National Institute of General Medical Sciences of the NIH. LBVW is supported by the NHLBI grant K23HL136891. The funders of this study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM
(PDF 462 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hatano, Y., VanWagner, L.B., Carnethon, M.R. et al. Racial difference in the association between non-alcoholic fatty liver disease and incident type 2 diabetes: findings from the CARDIA study. Diabetologia 66, 1235–1246 (2023). https://doi.org/10.1007/s00125-023-05903-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-023-05903-w