Abstract
Objective
This study aims to examine the ability of deep learning (DL)-derived imaging features for the prediction of radiation pneumonitis (RP) in locally advanced non-small-cell lung cancer (LA-NSCLC) patients.
Materials and methods
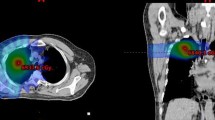
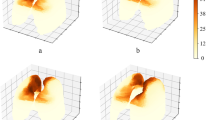
The study cohort consisted of 90 patients from the Fudan University Shanghai Cancer Center and 59 patients from the Affiliated Hospital of Jiangnan University. Occurrences of RP were used as the endpoint event. A total of 512 3D DL-derived features were extracted from two regions of interest (lung–PTV and PTV–GTV) delineated on the pre-radiotherapy planning CT. Feature selection was done using LASSO regression, and the classification models were built using the multilayered perceptron method. Performances of the developed models were evaluated by receiver operating characteristic curve analysis. In addition, the developed models were supplemented with clinical variables and dose–volume metrics of relevance to search for increased predictive value.
Results
The predictive model using DL features derived from lung–PTV outperformed the one based on features extracted from PTV–GTV, with AUCs of 0.921 and 0.892, respectively, in the internal test dataset. Furthermore, incorporating the dose–volume metric V30Gy into the predictive model using features from lung–PTV resulted in an improvement of AUCs from 0.835 to 0.881 for the training data and from 0.690 to 0.746 for the validation data, respectively (DeLong p < 0.05).
Conclusion
Imaging features extracted from pre-radiotherapy planning CT using 3D DL networks could predict radiation pneumonitis and may be of clinical value for risk stratification and toxicity management in LA-NSCLC patients.
Clinical relevance statement
Integrating DL-derived features with dose–volume metrics provides a promising noninvasive method to predict radiation pneumonitis in LA-NSCLC lung cancer radiotherapy, thus improving individualized treatment and patient outcomes.




Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- CNN:
-
Convolutional neural networks
- DL:
-
Deep learning
- DLR:
-
Deep learning-based radiomics
- GTV:
-
Gross tumor volume
- IMRT:
-
Intensity-modulated radiotherapy
- LA-NSCLC:
-
Locally advanced non-small-cell lung cancer
- LASSO:
-
Least absolute shrinkage and selection operator
- Lung–GTV:
-
Bilateral lung excluding GTV
- Lung–PTV:
-
Bilateral lung excluding PTV
- MLD:
-
Mean lung dose
- MLP:
-
Multilayered perceptron
- PTV:
-
Planning target volume
- ResNet:
-
Residual deep neural network
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- RP:
-
Radiation pneumonitis
- RTOG:
-
Radiation Therapy Oncology Group
- SBRT:
-
Stereotactic body radiotherapy
- SCC:
-
Squamous cell carcinoma
- SD:
-
Standard deviation
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Miller M, Hanna N (2021) Advances in systemic therapy for non-small cell lung cancer. BMJ 375:n2363. https://doi.org/10.1136/bmj.n2363
Keffer S, Guy CL, Weiss E (2020) Fatal radiation pneumonitis: literature review and case series. Adv Radiat Oncol 5:238–249. https://doi.org/10.1016/j.adro.2019.08.010
Graham MV, Purdy JA, Emami B, Harms W, Bosch W, Lockett MA et al (1999) Clinical dose-volume histogram analysis for pneumonitis after 3D treatment for non-small cell lung cancer (NSCLC). Int J Radiat Oncol Biol Phys 45:323–329. https://doi.org/10.1016/s0360-3016(99)00183-2
Tsujino K, Hirota S, Endo M, Obayashi K, Kotani Y, Satouchi M et al (2003) Predictive value of dose-volume histogram parameters for predicting radiation pneumonitis after concurrent chemoradiation for lung cancer. Int J Radiat Oncol Biol Phys 55:110–115. https://doi.org/10.1016/s0360-3016(02)03807-5
Katsui K, Ogata T, Watanabe K, Katayama N, Soh J, Kuroda M et al (2019) Dose-volume parameters predict radiation pneumonitis after induction chemoradiotherapy followed by surgery for non-small cell lung cancer: a retrospective analysis. BMC Cancer 19:1144. https://doi.org/10.1186/s12885-019-6359-9
Vogelius IR, Bentzen SM (2012) A literature-based meta-analysis of clinical risk factors for development of radiation induced pneumonitis. Acta Oncol 51:975–983. https://doi.org/10.3109/0284186X.2012.718093
Robnett TJ, Machtay M, Vines EF, McKenna MG, Algazy KM, McKenna WG (2000) Factors predicting severe radiation pneumonitis in patients receiving definitive chemoradiation for lung cancer. Int J Radiat Oncol Biol Phys 48:89–94. https://doi.org/10.1016/s0360-3016(00)00648-9
Hernando ML, Marks LB, Bentel GC, Zhou SM, Hollis D, Das SK et al (2001) Radiation-induced pulmonary toxicity: a dose-volume histogram analysis in 201 patients with lung cancer. Int J Radiat Oncol Biol Phys 51:650–659. https://doi.org/10.1016/s0360-3016(01)01685-6
Avanzo M, Stancanello J, Pirrone G, Sartor G (2020) Radiomics and deep learning in lung cancer. Strahlenther Onkol 196:879–887. https://doi.org/10.1007/s00066-020-01625-9
Kawahara D, Imano N, Nishioka R, Ogawa K, Kimura T, Nakashima T et al (2021) Prediction of radiation pneumonitis after definitive radiotherapy for locally advanced non-small cell lung cancer using multi-region radiomics analysis. Sci Rep 11:16232. https://doi.org/10.1038/s41598-021-95643-x
Krafft SP, Rao A, Stingo F, Briere TM, Court LE, Liao Z et al (2018) The utility of quantitative CT radiomics features for improved prediction of radiation pneumonitis. Med Phys 45:5317–5324. https://doi.org/10.1002/mp.13150
Huang B, Sollee J, Luo YH, Reddy A, Zhong Z, Wu J et al (2022) Prediction of lung malignancy progression and survival with machine learning based on pre-treatment FDG-PET/CT. EBioMedicine 82:104127. https://doi.org/10.1016/j.ebiom.2022.104127
Kuker RA, Lehmkuhl D, Kwon D, Zhao W, Lossos IS, Moskowitz CH et al (2022) A deep learning-aided automated method for calculating metabolic tumor volume in diffuse large B‑cell lymphoma. Cancers. https://doi.org/10.3390/cancers14215221
Yang F, Young LA, Johnson PB (2018) Quantitative radiomics: validating image textural features for oncological PET in lung cancer. Radiother Oncol 129:209–217. https://doi.org/10.1016/j.radonc.2018.09.009
Rich B, Huang J, Yang Y, Jin W, Johnson P, Wang L et al (2021) Radiomics predicts for distant metastasis in locally advanced human papillomavirus-positive oropharyngeal squamous cell carcinoma. Cancers. https://doi.org/10.3390/cancers13225689
Yang F, Thomas MA, Dehdashti F, Grigsby PW (2013) Temporal analysis of intratumoral metabolic heterogeneity characterized by textural features in cervical cancer. Eur J Nucl Med Mol Imaging 40:716–727. https://doi.org/10.1007/s00259-012-2332-4
Jiang W, Song Y, Sun Z, Qiu J, Shi L (2021) Dosimetric factors and radiomics features within different regions of interest in planning CT images for improving the prediction of radiation pneumonitis. Int J Radiat Oncol Biol Phys 110:1161–1170. https://doi.org/10.1016/j.ijrobp.2021.01.049
Chen S, Ma K, Zheng Y (2019) Med3D: transfer learning for 3D medical image analysis https://doi.org/10.48550/arXiv.1904.00625
Meng Y, Yang H, Wang W, Tang X, Jiang C, Shen Y et al (2019) Excluding PTV from lung volume may better predict radiation pneumonitis for intensity modulated radiation therapy in lung cancer patients. Radiat Oncol 14:7. https://doi.org/10.1186/s13014-018-1204-x
Okubo M, Itonaga T, Saito T, Shiraishi S, Mikami R, Nakayama H et al (2017) Predicting risk factors for radiation pneumonitis after stereotactic body radiation therapy for primary or metastatic lung tumours. Br J Radiol 90:20160508. https://doi.org/10.1259/bjr.20160508
Kumar G, Rawat S, Puri A, Sharma MK, Chadha P, Babu AG et al (2012) Analysis of dose-volume parameters predicting radiation pneumonitis in patients with esophageal cancer treated with 3D-conformal radiation therapy or IMRT. Jpn J Radiol 30:18–24. https://doi.org/10.1007/s11604-011-0002-2
Sheng L, Cui X, Cheng L, Chen Y, Du X (2019) Risk factors of grade ≥ 2 radiation pneumonitis after gemcitabine induction chemotherapy for patients with non-small cell lung cancer. Radiat Oncol 14:229. https://doi.org/10.1186/s13014-019-1440-8
Saha A, Beasley M, Hatton N et al (2021) Clinical and dosimetric predictors of radiation pneumonitis in early-stage lung cancer treated with Stereotactic ablative radiotherapy (SABR)—an analysis of UK’s largest cohort of lung SABR patients. Radiother Oncol 156:153–159. https://doi.org/10.1016/j.radonc.2020.12.015
Chetan MR, Gleeson FV (2021) Radiomics in predicting treatment response in non-small-cell lung cancer: current status, challenges and future perspectives. Eur Radiol 31:1049–1058. https://doi.org/10.1007/s00330-020-07141-9
Cunliffe A, Armato SG 3rd, Castillo R, Pham N, Guerrero T et al (2015) Lung texture in serial thoracic computed tomography scans: correlation of radiomics-based features with radiation therapy dose and radiation pneumonitis development. Int J Radiat Oncol Biol Phys 91:1048–1056. https://doi.org/10.1016/j.ijrobp.2014.11.030
Moran A, Daly ME, Yip SSF, Yamamoto T (2017) Radiomics-based assessment of radiation-induced lung injury after stereotactic body radiotherapy. Clin Lung Cancer 18:e425–e431. https://doi.org/10.1016/j.cllc.2017.05.014
Liang B, Tian Y, Chen X, Yan H, Yan L, Zhang T et al (2019) Prediction of radiation pneumonitis with dose distribution: a convolutional neural network (CNN) based model. Front Oncol 9:1500. https://doi.org/10.3389/fonc.2019.01500
Kapoor R, Sleeman W, Palta J, Weiss E (2023) 3D deep convolution neural network for radiation pneumonitis prediction following stereotactic body radiotherapy. J Appl Clin Med Phys 24:e13875. https://doi.org/10.1002/acm2.13875
Shah AA, Malik HAM, Muhammad A, Alourani A, Butt ZA (2023) Deep learning ensemble 2D CNN approach towards the detection of lung cancer. Sci Rep 13:2987. https://doi.org/10.1038/s41598-023-29656-z
Huang Y, Feng A, Lin Y, Gu H, Chen H, Wang H et al (2022) Radiation pneumonitis prediction after stereotactic body radiation therapy based on 3D dose distribution: dosiomics and/or deep learning-based radiomics features. Radiat Oncol 17:188. https://doi.org/10.1186/s13014-022-02154-8
Funding
1. Translational Medicine Project of Wuxi Commission of Health (grant no. ZH202101). 2. Top Talent Support Program for young and middle-aged people of Wuxi Health Committee (grant no. HB2023059). 3. Wuxi Translational Medical Research Institute Project Plan (grant no. LCYJ202339).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Y. Kong, M. Su, Y. Zhu, X. Li, J. Zhang, W. Gu, F. Yang, J. Zhou, J. Ni, X. Yang, Z. Zhu, and J. Huang declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors Yan Kong and Mingming Su have contributed equally to this work and share first authorship.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kong, Y., Su, M., Zhu, Y. et al. Enhancing the prediction of symptomatic radiation pneumonitis for locally advanced non-small-cell lung cancer by combining 3D deep learning-derived imaging features with dose–volume metrics: a two-center study. Strahlenther Onkol (2024). https://doi.org/10.1007/s00066-024-02221-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00066-024-02221-x