Abstract
Parkinson’s disease is second most common neurodegenerative disorder neurological illness that primarily affects patients in their later years of life. Specific neurons in the brain begin to malfunction resulting in a loss of a substance called dopamine which is characterized by the accumulation of α-synuclein aggregates within cells, forming structures known as Lewy bodies and Lewy neurites. It is affecting more than 1% of people worldwide (aged 65 and above) and is expected to increase in prevalence by 2030. Muscle rigidity, tremor, and unresponsiveness of motion are some of the motor signs of this condition, and on another hand pain, despair, and anxiety are some examples of non-motor symptoms. Levodopa, pramipexole, ropinirole, alprazolam, benztropine, trihexyphenidyl, and many more drugs are used to treat symptoms of Parkinson’s disease. Among them, the most common surgical symptomatic treatment is levodopa, which has better quality-of-life improvements in early Parkinson’s disease than other medications. Still, the success rate of medication is 14.9% only. Other than these patients are also treated with non-medications which are known as therapies like yoga, massage, music, and so on. As per the literature, most studies reveal that the therapies improved the quality of life by up to 58%. So, researchers need to be focused on the synthesis of novel drugs that create a high impact on the treatment of Parkinson’s disease. In this review paper, we discuss the pharmacological treatments for PD and discuss some of the current treatments. We hope this review article encourages the researchers to work in this field and develop new drugs against PD or permanent treatment for the person suffering from Parkinson.






Similar content being viewed by others
Abbreviations
- AD:
-
Alzheimer’s disease
- BBB:
-
blood-brain barrier
- COMT:
-
catechol-O-methyltransferase
- DA:
-
dopamine agonists
- FDA:
-
food and drug administration
- PD:
-
Parkinson disease
- L-DOPA:
-
levodopa
- LID:
-
levodopa induced dyskinesia’s
- MAO-B:
-
monoamine oxidative inhibitor
- NDRI:
-
norepinephrine and dopamine reuptake inhibitor
- NMS:
-
non-motor symptoms
- SN:
-
substantia nigra
- SNRI:
-
serotonin and norepinephrine reuptake inhibitor
- SSRI:
-
selective serotonin reuptake inhibitor
- UPDRS:
-
Unified Parkinson Disease Rating Scale
- UPR:
-
unfolded protein response.
References
Sveinbjornsdottir S. The clinical symptoms of Parkinson’s disease. J Neurochem. 2016;139:318–24. https://doi.org/10.1111/jnc.13691
Cacabelos R. Parkinson’s disease: from pathogenesis to pharmacogenomics. Int J Mol Sci. 2017;18:551. https://doi.org/10.3390/ijms18030551
Koszła O, Stępnicki P, Zięba A, Grudzińska A, Matosiuk D, Kaczor AA. Current approaches and tools used in drug development against parkinson’s disease. Biomolecules. 2021;11:1–16. https://doi.org/10.3390/biom11060897
Terashi H, Endo K, Kato H, Ido N, Aizawa H. Characteristics of sagittal spinopelvic alignment in patients with Parkinson’s disease. Acta Neurol Scand. 2022;145:53–62. https://doi.org/10.1111/ane.13521
Kimber TE. Approach to the patient with early Parkinson disease: diagnosis and management. Intern Med J. 2021;51:20–6. https://doi.org/10.1111/imj.15148
Sivanandy P, Leey TC, Xiang TC, Ling TC, Wey Han SA, Semilan SLA, et al. Systemic review on parkinson’s disease medications, emphasizing on three recently approved drugs to control parkinson’s symptoms. Int J Environ Res Public Health. 2022;19. https://doi.org/10.3390/ijerph19010364
Armstrong MJ, Okun MS. Diagnosis and treatment of Parkinson disease: a review. JAMA. 2020;323:548–60. https://doi.org/10.1001/jama.2019.22360
Tian Y, Chen R, Su Z. HMGB1 is a potential and challenging therapeutic target for Parkinson’s disease. Cell Mol Neurobiol. 2021;1:0123456789–58. https://doi.org/10.1007/s10571-021-01170-8
Rozpędek-Kamińska W, Siwecka N, Wawrzynkiewicz A, Wojtczak R, Pytel D, Diehl JA, et al. The PERK-dependent molecular mechanisms as a novel therapeutic target for neurodegenerative diseases. Int J Mol Sci. 2020;21:1–40. https://doi.org/10.3390/ijms21062108
Xu X, He X, Zhang Z, Chen Y, Li J, Ma S, et al. CREB inactivation by HDAC1/PP1c contributes to dopaminergic neurodegeneration in Parkinson’s disease. J Neurosci. 2022;42:4594–604. https://doi.org/10.1523/JNEUROSCI.1419-21.2022
Wittung-stafshede P. Gut power: modulation of human amyloid formation by amyloidogenic proteins in the gastrointestinal tract. Curr Opin Struct Biol. 2022;72:33–38. https://doi.org/10.1016/j.sbi.2021.07.009
Hansen CA, Miller DR, Annarumma S, Rusch CT, Ramirez-Zamora A, Khoshbouei H. Levodopa-induced dyskinesia: a historical review of Parkinson’s disease, dopamine, and modern advancements in research and treatment. J Neurol. 2022;269:2892–909. https://doi.org/10.1007/s00415-022-10963-w
Group PS. A controlled trial of rasagiline in early Parkinson disease. Arch Neurol. 2012;59:1937–43
Gallazzi M, Mauri M, Bianchi ML, Riboldazzi G, Princiotta Cariddi L, Carimati F, et al. Selegiline reduces daytime sleepiness in patients with Parkinson’s disease. Brain Behav. 2021;11:1–5. https://doi.org/10.1002/brb3.1880
Meira B, Degos B, Corsetti E, Doulazmi M, Berthelot E, Virbel-Fleischman C, et al. Long-term effect of apomorphine infusion in advanced Parkinson’s disease: a real-life study. npj Parkinson’s Dis. 2021;7:50–61. https://doi.org/10.1038/s41531-021-00194-7
Cennamo M, Dragotto F, Favuzza E, Morelli A, Mencucci R. Amantadine therapy for Parkinson’s Disease: In Vivo Confocal Microscopy corneal findings, case report and revision of literature. BMC Ophthalmol. 2022;22:1–5. https://doi.org/10.1186/s12886-022-02410-1
Li B, Yang Y, Wang Y, Zhang J, Ding J, Liu X, et al. Acetylation of NDUFV1 induced by a newly synthesized HDAC6 inhibitor HGC rescues dopaminergic neuron loss in Parkinson models. Science. 2021;24:102302 https://doi.org/10.1016/j.isci.2021.102302
Layton JB, Forns J, Turner ME, Dempsey C, Bartsch JL, Anthony MS, et al. Falls and fractures in patients with Parkinson’s disease-related psychosis treated with Pimavanserin vs atypical antipsychotics: a cohort study. Drugs – Real World Outcomes. 2022;9:9–22. https://doi.org/10.1007/s40801-021-00284-1
Zhang X, Che C. Drug repurposing for Parkinson’s disease by integrating knowledge graph completion model and knowledge fusion of medical literature. Future Internet. 2021;13:1–13. https://doi.org/10.3390/fi13010014
Reddy DH, Misra S, Medhi B. Advances in drug development for Parkinson’s disease: present status. Pharmacology. 2014;93:260–71. https://doi.org/10.1159/000362419
James JH, Beck C. The silver book: Parkinson’s disease. Chronic disease and medical innovation in an aging nation. Alliance for Aging Research; 2019
Ray Dorsey E, Elbaz A, Nichols E, Abd-Allah F, Abdelalim A, Adsuar JC, et al. Global, regional, and national burden of Parkinson’s disease, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:939–53. https://doi.org/10.1016/S1474-4422(18)30295-3
Soto-Lara M, Silva-Loredo M, Monroy-Córdoba JR, Flores-Ordoñez P, Cervera-Delgadillo NG, Carrillo-Mora P. Alternative medicine therapies in neurological disorders: prevalence, reasons and associated factors. A systematic review. Complement Ther Med. 2023;73:0–2. https://doi.org/10.1016/j.ctim.2023.102932
Carter AM, Dioso ER, Romero B, Clinker CE, Lucke-Wold B. Complementary medicine and expressive arts therapy: adjuvant for recovery following neurosurgical procedures. OBM Integr Complement Med. 2023;08:1–14. https://doi.org/10.21926/obm.icm.2301007
Jang JH, Kim J, Kwon O, Jung SY, Lee HJ, Cho SY, et al. Effectiveness and therapeutic mechanism of pharmacopuncture for pain in Parkinson’s disease: a study protocol for a pilot pragmatic randomized, assessor-blinded, usual care-controlled, three-arm parallel trial. Int J Environ Res Public Health. 2023;20. https://doi.org/10.3390/ijerph20031776
Calderone A, Formenti M, Aprea F, Papa M, Alberghina L, Colangelo AM, et al. Comparing Alzheimer’s and Parkinson’s diseases networks using graph communities structure. BMC Syst Biol. 2016;10:1–10. https://doi.org/10.1186/s12918-016-0270-7
Eliewi AG, Al-Garawi ZS, Al-Kazzaz FF, Atia AJK. Multi target-directed imidazole derivatives for neurodegenerative diseases. J Phys Conf Ser. 2021;1853:0–17. https://doi.org/10.1088/1742-6596/1853/1/012066
Düzel E, Costagli M, Donatelli G, Speck O, Cosottini M. Studying Alzheimer disease, Parkinson disease, and amyotrophic lateral sclerosis with 7-T magnetic resonance. Eur Radiol Exp. 2021;5:36 https://doi.org/10.1186/s41747-021-00221-5
Mcgirr S, Venegas C, Swaminathan A. Alzheimer’s disease: a brief review. J Exp Neurol. 2020;1:89–98. https://doi.org/10.33696/Neurol.1.015
Marie L. Parkinson’s dementia. The complete guide for people with Parkinson’s disease and their loved ones. 2020. 175–6. https://doi.org/10.2307/j.ctv15wxntx.61
Biswas AK, Das S. Alzheimer and Parkinson’s disease—two faces of the same disease? J Alzheimer’s Dis Parkinson. 2016. 06. https://doi.org/10.4172/2161-0460.1000222
Tamara P, Day GS, Smith DB, Rae-Grant A, Licking N, Armstrong MJ, et al. Dopaminergic therapy for motor symptoms in early Parkinson disease practice Guideline summary. Neurology. 2021;97:942–57. https://doi.org/10.1212/wnl.0000000000012868
Kouli A, Torsney KM, Kuan W-L. Parkinson’s disease: etiology, neuropathology, and pathogenesis. Codon Publications. 2018:3–26. https://doi.org/10.15586/codonpublications.parkinsonsdisease.2018
Xia R, Mao ZH. Progression of motor symptoms in Parkinson’s disease. Neurosci Bull. 2012;28:39–48. https://doi.org/10.1007/s12264-012-1050-z
Höglund A, Hagell P, Broman JE, Pålhagen S, Sorjonen K, Fredrikson S, et al. Associations between fluctuations in daytime sleepiness and motor and non-motor symptoms in Parkinson’s disease. Mov Disord Clin Pract. 2021;8:44–50. https://doi.org/10.1002/mdc3.13102
Dong J, Cui Y, Li S, Le W. Current pharmaceutical treatments and alternative therapies of Parkinson’s disease. Curr Neuropharmacol. 2016;14:339–55. https://doi.org/10.2174/1570159x14666151120123025
Review N, Start WTO, Treatment S, Schapira AHV. Treatment options in the modern management of Parkinson disease. Arch Neurol. 2007;64:1083–8. https://doi.org/10.1001/archneur.64.8.1083
Kumaresan M, Khan S. Spectrum of non-motor symptoms in Parkinson’s disease. Cureus. 2021;13. https://doi.org/10.7759/cureus.13275
Sang Q, Liu X, Wang L, Qi L, Sun W, Wang W, et al. CircSNCA downregulation by pramipexole treatment mediates cell apoptosis and autophagy in Parkinson’s disease by targeting miR-7. Aging. 2018;10:1281–93. https://doi.org/10.18632/aging.101466
AlDakheel A, Kalia LV, Lang AE. Pathogenesis-targeted, disease-modifying therapies in Parkinson disease. Neurotherapeutics. 2014;11:6–23. https://doi.org/10.1007/s13311-013-0218-1
Cuervo AM, Stafanis L, Fredenburg R, Lansbury PT, Sulzer D. Impaired degradation of mutant α-synuclein by chaperone-mediated autophagy. Science. 2004;305:1292–5. https://doi.org/10.1126/science.1101738
Paillusson S, Gomez-Suaga P, Stoica R, Little D, Gissen P, Devine MJ, et al. α-Synuclein binds to the ER–mitochondria tethering protein VAPB to disrupt Ca2+ homeostasis and mitochondrial ATP production. Acta Neuropathol. 2017;134:129–49. https://doi.org/10.1007/s00401-017-1704-z
Elkouzi A, Vedam-Mai V, Eisinger RS, Okun MS. Emerging therapies in Parkinson disease—repurposed drugs and new approaches. Nat Rev Neurol. 2019;15:204–23. https://doi.org/10.1038/s41582-019-0155-7
Ovallath S, Sulthana B. Levodopa: history and therapeutic applications. Ann Indian Acad Neurol. 2017;20:185–9. https://doi.org/10.4103/aian.AIAN_241_17
Goldenberg MM. Medical management of Parkinson’s disease. Pharm Ther. 2008;33:590–6
Rao SK, Vakil SD, Calne DB, Hilson A, Rao SK, Lond D, et al. Augmenting the action of levodopa. Postgrad Med J. 1972;48:653–6. https://doi.org/10.1136/pgmj.48.565.653
Ansari AJ, Khushtar M, Fatima N, Monawwar MT, Alhamd Khan MF. An overview on the diagnosis and approaches in pharmacological management of Parkinson’s disease. Res Rev J Neurosci. 2021;11:1–8. https://doi.org/10.37591/RRJoNS
Connolly BS, Lang AE. Pharmacological treatment of Parkinson disease: a review. JAMA. 2014;311:1670–83. https://doi.org/10.1001/jama.2014.3654
Wojciech DP, Dekundy A, Scheschonka A, Riederer P. Amantadine: reappraisal of the timeless diamond—target updates and novel therapeutic potentials. J Neural Transm. 2021;128:127–69. https://doi.org/10.1007/s00702-021-02306-2
Hauser RA, Walsh RR, Pahwa R, Chernick D, Formella AE. Amantadine ER (Gocovri®) significantly increases on time without any dyskinesia: pooled analyses from pivotal trials in Parkinson’s disease. Front Neurol. 2021;12:1–9. https://doi.org/10.3389/fneur.2021.645706
Crosby NJ, Deane K, Clarke CE. Amantadine for dyskinesia in Parkinson’s diseas. Cochrane Database Syst Rev. 2003;2010:003467 https://doi.org/10.1002/14651858.CD003467
Hauser RA, Lytle J, Formella AE, Tanner CM. Amantadine delayed release/extended release capsules significantly reduce OFF time in Parkinson’s disease. npj Parkinson’s Dis. 2022;8:29–36. https://doi.org/10.1038/s41531-022-00291-1
Rascols O, Tönges L, deVries T, Jaros M, Quartel A, Jacobs D, et al. Immediate-release/extended-release amantadine (OS320) to treat Parkinson’s disease with levodopa-induced dyskinesia: Analysis of the randomized, controlled ALLAY-LID studies. Parkinsonism Relat Disord. 2022;96:65–73. https://doi.org/10.1016/j.parkreldis.2022.01.022
Borkar N, Mu H, Holm R. Challenges and trends in apomorphine drug delivery systems for the treatment of Parkinson’s disease. Asian J Pharm Sci. 2018;13:507–17. https://doi.org/10.1016/j.ajps.2017.11.004
Carbone F, Djamshidian A, Seppi K, Poewe W. Apomorphine for Parkinson’s disease: efficacy and safety of current and new formulation. CNS Drugs. 2019;33:905–18. https://doi.org/10.1007/s40263-019-00661-z
Antonini A, Jenner P. Apomorphine infusion in advanced Parkinson disease. Nat Rev Neurol. 2018;14:693–4. https://doi.org/10.1038/s41582-018-0083-y
Christensen PB, Dupont E, Jensen NB. Apomorphine in the treatment of Parkinson disease. Ugeskr Laege. 1991;153:2631–4.
Cheer GM, Bang SM, Keating LM. Ropinirole: for the treatment of restless legs syndrome. CNS Drugs. 2004;18:747–54. https://doi.org/10.2165/00023210-200418110-00004
Silva S, Almeida AJ, Vale N. Importance of nanoparticles for the delivery of antiparkinsonian drugs. Pharmaceutics. 2021;13:508 https://doi.org/10.3390/pharmaceutics13040508
Shill HA, Stacy M. Update on ropinirole in the treatment of Parkinson’s disease. Neuropsychiatr Dis Treat. 2009;5:33–36. https://doi.org/10.2147/ndt.s3237
Nashatizadeh MM, Lyons KE, Pahwa R. A review of ropinirole prolonged release in Parkinson’s disease. Clin Interv Aging. 2009;4:179–86. https://doi.org/10.2147/cia.s3358
Zhang J, Gao X, Chen Y, Kong Q. Clinical observation of ropinirole hydrochloride in the treatment of Parkinson’s disease. Comput Math Methods Med. 2022;2022:1–7. https://doi.org/10.1155/2022/3989770
Tábi T, Vécsei L, Youdim MB, Riederer P, Szökő É. Selegiline: a molecule with innovative potential. J Neural Transm. 2020;127:831–42. https://doi.org/10.1007/s00702-019-02082-0
Jost WH. A critical appraisal of MAO-B inhibitors in the treatment of Parkinson’s disease. J Neural Transm. 2022;129:723–36. https://doi.org/10.1007/s00702-022-02465-w
Bali N, Salve PS. Fabrication and evaluation of selegiline HCl embedded transdermal film for management of Parkinson’s disease. J Drug Deliv Ther. 2019;9:344–51. https://doi.org/10.22270/jddt.v9i2.2577
Magyar K. The pharmacology of selegiline. Int Rev Neurobiol. 2011;100:65–84. https://doi.org/10.1016/B978-0-12-386467-3.00004-2
Robakis D, Fahn S. Defining the role of the monoamine oxidase-B inhibitors for Parkinson’s disease. CNS Drugs. 2015;29:433–41. https://doi.org/10.1007/s40263-015-0249-8
Lecht S, Haroutiunian S, Hoffman A, Lazarovici P. Rasagiline—a novel MAO B inhibitor in Parkinson’s disease therapy. Ther Clin Risk Manag. 2007;3:467–74
Hudry J, Rinne JO, Keränen T, Eckert L, Cochran JM. Cost-utility model of Rasagiline in the treatment of advanced Parkinson’s disease in Finland. Ann Pharmacother. 2006;40:651–7. https://doi.org/10.1345/aph.1G454
Kano O, Ikeda K, Kiyozuka T, Iwamoto K, Ito H, Kawase Y, et al. Beneficial effect of pramipexole for motor function and depression in Parkinson’s disease. Neuropsychiatr Dis Treat. 2008;4:707–10. https://doi.org/10.2147/ndt.s2921
Wolfram E, Sommer B, Hartter S, Jost WH. Pramipexole extended release: a novel treatment option in Parkinson’s disease. Parkinson’s Dis. 2010;2010:612619 https://doi.org/10.4061/2010/612619
Hauser RA, Giladi N, Poewe W, Brotchie J, Friedman H, Oren S, et al. P2B001 (extended release pramipexole and rasagiline): a new treatment option in development for Parkinson’s disease. Adv Ther. 2022;39:1881–94. https://doi.org/10.1007/s12325-022-02097-2
McAfee DA, Hadgraft J, Lane ME. Rotigotine: the first new chemical entity for transdermal drug delivery. Eur J Pharm Biopharm. 2014;88:586–93. https://doi.org/10.1016/j.ejpb.2014.08.007
Ouchi M, Kitta T, Chiba H, Higuchi M, Togo M, Abe-Takahashi Y, et al. Mechanisms of D1/D2-like dopaminergic agonist, rotigotine, on lower urinary tract function in rat model of Parkinson’s disease. Sci Rep. 2022;12:1–8. https://doi.org/10.1038/s41598-022-08612-3
Raeder V, Boura I, Leta V, Jenner P, Reichmann H, Trenkwalder C, et al. Rotigotine transdermal patch for motor and non-motor parkinson’s disease: a review of 12 years’ clinical experience. CNS Drugs. 2021;35:215–31. https://doi.org/10.1007/s40263-020-00788-4
Yeni Y, Wu X, Arman B. Anti-Parkinson drug from chemical medicines and herbal medicines: a review. Pharm Biomed Sci J 2022;3:45–58. https://doi.org/10.15408/pbsj.v3i1.20304
Benitez A, Edens H, Fishman J, Moran K, Asgharnejad M. Rotigotine transdermal system: developing continuous dopaminergic delivery to treat Parkinson’s disease and restless legs syndrome. Ann NY Acad Sci. 2014;1329:45–66. https://doi.org/10.1111/nyas.12508
Schrag A. Entacapone in the treatment of Parkinson’s disease. Lancet Neurol. 2005;4:366–70. https://doi.org/10.1016/S1474-4422(05)70098-3
Jo M, Palma PN. Catechol-O-methyltransferase and Its Inhibitors in Parkinson’s disease. CNS Drug Rev. 2007;13:352–79. https://doi.org/10.1007/s40265-014-0343-0
Salamon A, Zádori D, Szpisjak L, Klivényi P, Vécsei L. What is the impact of catechol-O-methyltransferase (COMT) on Parkinson’s disease treatment? Expert Opin Pharmacother. 2022;1:1123–8. https://doi.org/10.1080/14656566.2022.2060738
Rizek SJ, Kumar P, Mandar N. An update on the diagnosis and treatment of Parkinson’s disease. CMAJ. 2016;188:1157–65. https://doi.org/10.1503/cmaj.151179
Artusi CA, Sarro L, Imbalzano G, Fabbri M, Lopiano L. Safety and efficacy of tolcapone in Parkinson’s disease: systematic review. Eur J Clin Pharmacol. 2021;77:817–29. https://doi.org/10.1007/s00228-020-03081-x
Saeedi Y, Ghadimi M, Rohani M, Emamikhah M, Shahidi G, Moghaddasi M, et al. Impact of anticholinergic drugs withdrawal on motor function in patients with Parkinson’s disease. Clin Neurol Neurosurg. 2021;202:106480 https://doi.org/10.1016/j.clineuro.2021.106480
Zhao J, Xu G, Feng C, Chen Y, Kang Y, Liu F, et al. Trihexyphenidyl induced malignant hyperthermia in a patient with Parkinson’s disease complicated with pneumonia: a case report. Medicines. 2020;99:2019–21. https://doi.org/10.1097/MD.0000000000020129
Teixeira FG, Gago MF, Marques P, Moreira PS, Magalhães R, Sousa N, et al. Safinamide: a new hope for Parkinson’s disease? Drug Discov Today. 2018;23:736–44. https://doi.org/10.1016/j.drudis.2018.01.033
Wasan H, Singh D, KH R. Safinamide in neurological disorders and beyond: evidence from preclinical and clinical studies. Brain Res Bull. 2021;168:165–77. https://doi.org/10.1016/j.brainresbull.2020.12.018
Giossi R, Carrara F, Mazzari M, Lo Re F, Senatore M, Schicchi A, et al. Overall efficacy and safety of safinamide in Parkinson’s disease: a systematic review and a meta-analysis. Clin Drug Investig. 2021;41:321–39. https://doi.org/10.1007/s40261-021-01011-y
Valldeoriola F, Grandas F, Arbelo JM, Blázquez Estrada M, Calopa Garriga M, Campos-Arillo VM, et al. Spanish expert consensus on the use of safinamide in Parkinson’s disease. Neurolía. 2021;36:666–72. https://doi.org/10.1016/j.nrleng.2018.04.004
Sanger GJ, Andrews PLR. A history of drug discovery for treatment of nausea and vomiting and the implications for future research. Front Pharmacol. 2018;9:1–35. https://doi.org/10.3389/fphar.2018.00913
Ye J, Hong P, Rex Schaefer R. Ondansetron: a selective 5-HT3 receptor antagonist and its applications in CNS-related disorders. CNS Drug Rev. 2001;7:199–13. https://doi.org/10.1111/j.1527-3458.2001.tb00195.x
Tsitsipa E, Rogers J, Casalotti S, Belessiotis-Richards C, Zubko O, Weil RS, et al. Selective 5HT3 antagonists and sensory processing: a systematic review. Neuropsychopharmacology. 2022;47:880–90. https://doi.org/10.1038/s41386-021-01255-4
Butler A, Hill JM, Ireland SJ, Jordan CC, Tyers MB. Pharmacological properties of GR38032F, a novel antagonist at 5‐HT3 receptors. Br J Pharmacol. 1988;94:397–12. https://doi.org/10.1111/j.1476-5381.1988.tb11542.x
Stern ER, Shahab R, Grimaldi SJ, Leibu E, Murrough JW, Fleysher L, et al. High-dose ondansetron reduces activation of interoceptive and sensorimotor brain regions. Neuropsychopharmacology. 2019;44:390–8. https://doi.org/10.1038/s41386-018-0174-x
Leeser J, Lip H. Prevention of postoperative nausea and vomiting using ondansetron, a new, selective, 5-HT3 receptor antagonist. Anesth Analg. 1991;72:751–5. https://doi.org/10.1213/00000539-199106000-00005
Shin H-J, Koo B-W, Yoon J, Kim H, Do S-H, Na H-S. Melatonin reduces the endoplasmic reticulum stress and polyubiquitinated protein accumulation induced by repeated anesthesia exposure in Caenorhabditis elegans. Sci Rep. 2022;12:1–8. https://doi.org/10.1038/s41598-022-09853-y
Mack JM, Schamne MG, Sampaio TB, Pértile RAN, Fernandes PACM, Markus RP, et al. Melatoninergic system in Parkinson’s disease: from neuroprotection to the management of motor and nonmotor symptoms. Oxid Med Cell Longev. 2016. https://doi.org/10.1155/2016/3472032
Farnoosh G, Akbariqomi M, Badri T, Bagheri M, Izadi M. Efficacy of a low dose of melatonin as an adjunctive therapy in hospitalized patients with COVID-19: a randomized, double-blind clinical trial. Arch Med Res. 2022;53:79–85. https://doi.org/10.1016/j.arcmed.2021.06
Jiménez-Delgado A, Ortiz GG, Delgado-Lara DL, González-Usigli HA, González-Ortiz LJ, Cid-Hernández M, et al. Effect of melatonin administration on mitochondrial activity and oxidative stress markers in patients with Parkinson’s disease. Oxid Med Cell Longev. 2021. https://doi.org/10.1155/2021/5577541
Sakellaropoulou A, Siamidi A. Melatonin/cyclodextrin inclusion complexes: a review. Molecules. 2022;27:445–60. https://doi.org/10.3390/molecules27020445
Bruni O, Alonso-Alconada D, Besag F, Biran V, Braam W, Cortese S, et al. Current role of melatonin in pediatric neurology: clinical recommendations. Eur J Paediatr Neurol. 2015;19:122–33. https://doi.org/10.1016/j.ejpn.2014.12.007
Perez-Caballero L, Torres-Sanchez S, Bravo L, Mico JA, Berrocoso E. Fluoxetine: a case history of its discovery and preclinical development. Expert Opin Drug Discov. 2014;9:567–78. https://doi.org/10.1517/17460441.2014.907790
Mostert JP, Koch MW, Heerings M, Heersema DJ, De Keyser J. Therapeutic potential of fluoxetine in neurological disorders. CNS Neurosci Ther. 2008;14:153–64. https://doi.org/10.1111/j.1527-3458.2008.00040.x
Hippius H. A historical perspective of clozapine. J Clin Psychiatry. 1999;60:22–3
Gammon D, Cheng C, Volkovinskaia A, Baker GB, Dursun SM. Clozapine: why is it so uniquely effective in the treatment of a range of neuropsychiatric disorders? Biomolecules. 2021;11:1–19. https://doi.org/10.3390/biom11071030
Fitzgerald RL, Herold DA. Improved CEDIA® benzodiazepine assay eliminates sertraline crossreactivity. J Anal Toxicol. 1997;21:32–35. https://doi.org/10.1093/jat/21.1.32
Dadić-Hero E, Ružić K, Grahovac T, Graovac M, Palijan TŽ, Šepić-Grahovac D. Allergic reactions—outcome of sertraline and escitalopram treatments. Psychiatr Danubina. 2011;23:120–2
Latorre MA, Pina Modrego PJ, Rodilla F, Catalán C, Calvo M. Parkinsonism and Parkinson’s disease associated with long-term administration of sertraline. J Clin Pharm Ther. 2001;26:111–2. https://doi.org/10.1046/j.1365-2710.2001.00307.x
Huot P, Fox SH, Brotchie JM. Monoamine reuptake inhibitors in Parkinson’s disease. Parkinson’s Dis. 2015;2015:609428 https://doi.org/10.1155/2015/609428
Kowalska M, Nowaczyk J, Fijałkowski Ł, Nowaczyk A. Paroxetine—overview of the molecular mechanisms of action. Int J Mol Sci. 2021;22:1–21. https://doi.org/10.3390/ijms22041662
Gupta A, Sharma V, Singh L. Devastating depression of youth and its remedial drug: a review. Eur J Biomed Pharm Sci. 2018;5:962–71.
Vismara M, Benatti B, Nicolini G, Cova I, Monfrini E, Di Fonzo A, et al. Clinical uses of Bupropion in patients with Parkinson’s disease and comorbid depressive or neuropsychiatric symptoms: a scoping review. BMC Neurol. 2022;22:1–20. https://doi.org/10.1186/s12883-022-02668-4
Raskin S, Durst R. Bupropion as the treatment of choice in depression associated with Parkinson’s disease and it’s various treatments. Med Hypotheses. 2010;75:544–6. https://doi.org/10.1016/j.mehy.2010.07.024
Stahl SM, Pradko JF, Haight BR, Modell JG, Rockett CB, Learned Coughlin S. A review of the neuropharmacology of bupropion, a dual norepinephrine and dopamine reuptake inhibitor. Prim Care Companion J Clin Psychiatry. 2004;06:159–66. https://doi.org/10.4088/pcc.v06n0403
Peña E, Mata M, López-Manzanares L, Kurtis M, Eimil M, Martínez-Castrillo JC, et al. Antidepressants in Parkinson’s disease. Recommendations by the movement disorder study group of the Neurological Association of Madrid. Neurolía (Engl Ed). 2018;33:395–402. https://doi.org/10.1016/j.nrleng.2016.02.017
Váradi C. Clinical features of Parkinson’s disease. Biology. 2020;9:103–16. https://doi.org/10.1002/9783527629480.ch2
Werner P, Antonini A, Zijlmans JC, Burkhard PR, Vingerhoets F. Levodopa in the treatment of Parkinson’s disease: an old drug still going strong. Clin Interv Aging. 2010;5:229–38. https://doi.org/10.2147/cia.s6456
Hou JGG, Lai EC. Non-motor symptoms of Parkinson’s disease. Int J Gerontol. 2007;1:53–64. https://doi.org/10.1016/S1873-9598(08)70024-3
Habet S. The clinical pharmacology of entacapone (Comtan®) from the Food and Drug Administration (FDA) reviewer. Int J Neuropsychopharmacol. 2022;1–9. https://doi.org/10.1093/ijnp/pyac021
Anttila EVJ, Leinonen SAK. A review of the pharmacological and clinical profile of mirtazapine. CNS Drug Rev. 2001;7:249–64. https://doi.org/10.1111/j.1527-3458.2001.tb00198.x
Acknowledgements
The authors are highly thankful to Chandigarh University, Gharuan for providing basic facility to write the review article.
Author information
Authors and Affiliations
Contributions
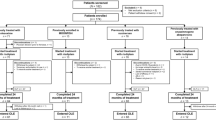
NS, MK, and HSS conceived the review. NS drafted the manuscript and shared the first authorship. NS, AM, MV, SG and KS collected the data. AM, KS, and MK analyzed the data and made tables. NS and HSS made the figures.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Saini, N., Singh, N., Kaur, N. et al. Motor and non-motor symptoms, drugs, and their mode of action in Parkinson’s disease (PD): a review. Med Chem Res 33, 580–599 (2024). https://doi.org/10.1007/s00044-024-03203-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00044-024-03203-5